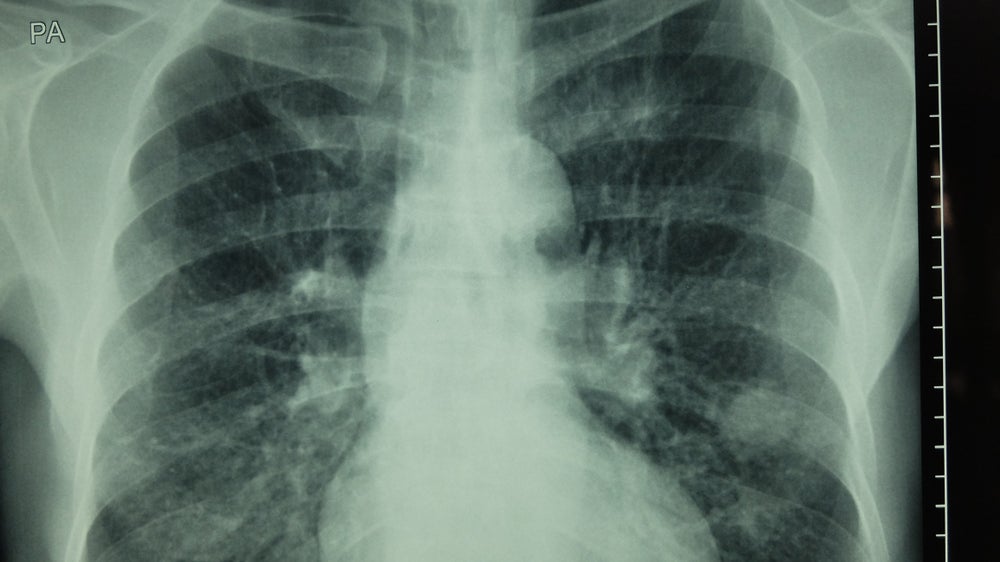
Janssen’s Rybrevant (amivantamab-vmjw)/lazertinib combination data has prompted expert discussion on whether Rybrevant alone could hold future utility in non-small cell lung cancer (NSCLC) after AstraZeneca’s Tagrisso (osimertinib). However, activity against brain metastases favors the former. Regardless, both the Rybrevant/lazertinib combination and Daiichi Sankyo’s Her3-DXd (patritumab deruxtecan) each signal potential for inclusion into standard of care (SOC) in NSCLC.
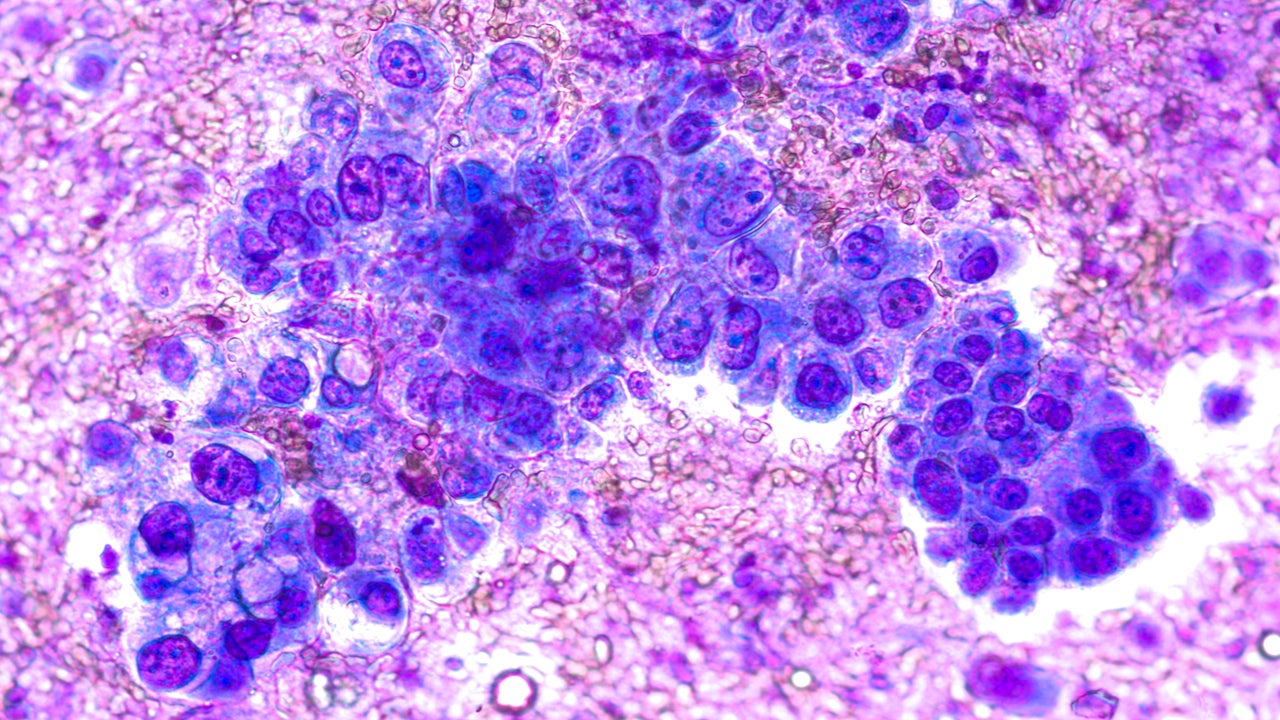
The therapies tested in EGFR-mutated NSCLC posted roughly comparable activities at the recent American Society of Clinical Oncology (ASCO) annual meeting. Experts said the presentations were two of the most significant ones in NSCLC, indicating a likely inclusion into the armamentarium once additional randomized data from larger studies is collected. Considering Tagrisso’s place as a prominent first-line (1L) therapy, treatment after relapse on Tagrisso is a major unmet need, experts said.
Given clinical data from a past study, some experts said Rybrevant monotherapy carried potential utility and would reduce the toxicity burden and financial costs compared to a combination. But experts highlighted the lack of updated Rybrevant monotherapy data which made its potential for off-label use in this setting less likely. Also, others said lazertinib’s inclusion is necessary to address central nervous system (CNS) metastases. This would be especially significant in the 1L setting, where the combination is also being tested in a Phase III trial in comparison to Tagrisso.
Janssen’s clinical program is currently focused on studying Rybrevant in combination with lazertinib in the post-Tagrisso setting, said a spokesperson.
In terms of patritumab deruxtecan, Phase I (NCT03260491) efficacy data bodes well for its use, experts said. Nonetheless, data thus far did not provide any clear benefit to either Rybrevant/lazertinib or patritumab deruxtecan in terms of a competitive profile. While this efficacy—an overall response rate (ORR) of 30%–40%—with both therapies is also comparable to chemotherapy, which is standard in this setting, a targeted approach aided by biomarkers offers potential for better duration of response (DOR). If anything, the antibody-drug conjugate’s (ADC) safety profile may be scrutinized given the association of ADCs with pneumonitis or lung toxicities in other cancers. This toxicity will be particularly relevant in NSCLC and could help drive treatment choice.
Rybrevant, manufactured by The Janssen Pharmaceutical Companies of Johnson & Johnson, was granted an accelerated approval last month as a monotherapy for patients with NSCLC with EGFR exon 20 insertion mutations after progression on or after chemotherapy. Rybrevant and lazertinib are estimated to make $378m and $569m in 2029, respectively, as per GlobalData consensus forecasts. J&J’s market cap is $431.93bn. Patritumab deruxtecan is expected to yield $750m in 2027. Daiichi’s market cap is JPY4.66trn.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
By GlobalDataCombo shows efficacy, but Rybrevant monotherapy potential piques interest
The take-home message with the Rybrevant/lazertinib data is that the combination’s benefit is seen across all-comers, but some subsets may benefit more, said Dr Alex Spira, medical oncologist, Virginia Cancer Specialists, Fairfax. In the Phase I CHRYSALIS study (NCT02609776), a response rate of 36% was noted in 45 Tagrisso-relapsed, chemotherapy-naive EGFR-mutated NSCLC patients with a median progression-free survival (PFS) of 4.9 months (abstract no 9006).
However, most of the efficacy benefit could likely be coming from Rybrevant alone, said Dr Balazs Halmos, director of the Multidisciplinary Thoracic Oncology Program, Montefiore Health Systems, New York. Previously, efficacy signals were also seen with Rybrevant alone, so it is unclear if combination is better than monotherapy, said Dr Timothy Burns, medical oncologist, University of Pennsylvania Medical Center Hillman Cancer Center, Pittsburgh. In a 2019 ASCO update, with Rybrevant monotherapy in EGFR-mutated patients relapsed on third-generation tyrosine kinase inhibitors (TKIs) and EGFR exon 20 disease, 25/88 (28%) achieved a best timepoint response of partial response (PR) (Haura et al, Journal of Clinical Oncology 37, no. 15_suppl (May 20, 2019)).
Whether lazertinib is required for efficacy is a question, but the combination data is still early and does not have enough patients to draw any conclusions, said Burns and Dr Nathan Pennell, professor of medicine, Cleveland Clinic Lerner College of Medicine, Ohio. If Rybrevant could be used alone, it would be less toxic and expensive, said Pennell. In this post-Tagrisso setting, the first choice would still be chemotherapy or participating in a clinical trial, but more monotherapy data could be instructive before considering off-label use, said Pennell.
However, the big concern with using Rybrevant alone is that it may not have CNS penetration, and lazertinib could address that, said Spira and Halmos. The combination could allow sustained CNS activity, which is a key component as this combination is also studied in 1L, Halmos added. Theoretically, the combination in 1L should also reduce the possibility of resistance and increase the DOR, said Dr Nicola Normanno, chief, Cell Biology and Biotherapy Unit, INT-Fondazione Pascale, Naples, Italy, but more data is needed. A 1,000-patient Phase III study titled MARIPOSA (NCT04487080) is testing the Rybrevant/lazertinib combination against Tagrisso as a first-line therapy in EGFR-mutated NSCLC.
Also, targeting the same EGFR pathway through two different mechanisms, the kinase activity with lazertinib and its EGFR expression levels with Rybrevant, may be particularly beneficial in terms of efficacy, said Burns.
Patritumab deruxtecan efficacy across all-comers
Like the combination, experts were encouraged by patritumab deruxtecan’s efficacy profile. An ORR of 39% was recorded, with 57 patients treated with patritumab deruxtecan with a median DOR of 6.9 months (abstract no 9007). There was no clear benefit with the ADC observed based on a biomarker, said Pennell.
In CHRYSALIS, 17 of the 45 patients had EGFR/MET-based resistance as identified by NGS, and the ORR in this subgroup was 47% and mDOR was 10.4 months. Both Pennell and Dr Frank Griesinger, director, Department of Internal Medicine-Oncology, Pius Hospital, Medizinischer Campus, Universität Oldenverg, Germany, noted that this could be a potential subset to target.
However, neither of these therapies posted a high ORR of 60–70%, which has been seen for other drugs in NSCLC, said Burns and Pennell. With both approaches, however, targeting individual biomarker-based populations would ideally allow higher efficacy, said Pennell. Identifying potential subsets is relevant but small patient numbers make it difficult to rule out heterogeneity or selection bias, said Griesinger. Patritumab deruxtecan’s efficacy was observed in patients with and without known EGFR TKI resistance mechanisms in a population that is often difficult to treat, said a Daiichi Sankyo spokesperson.
While the DOR with these therapies is probably longer than chemotherapy, the existing data is inadequate to know whether this can be used in lieu of chemotherapy yet, said Spira and Halmos. Chemotherapy is SOC after Tagrisso, but patients do not prefer it due to its toxicity profile, said Halmos. In addition to the aforementioned study, patritumab deruxtecan is also being evaluated in a Phase Ib study (NCT04676477) in combination with Tagrisso for patients with EGFR-mutated metastatic NSCLC who have progressed after Tagrisso, the spokesperson noted.
Managing toxicities like pneumonitis may be key
There is no dramatic toxicity associated with the Rybrevant/lazertinib combination and it can be given at the maximum tolerated dose without the need to adjust the dose significantly, said Spira. With the combination, the most common adverse events (AE) were infusion-related reactions (IRR) in 78% of patients and rash, which included acneiform dermatitis and rash, in 51% and 27% of patients, respectively. Infusion reactions with Rybrevant monotherapy do improve but need to be monitored, said Burns. The Rybrevant monotherapy question is also relevant because there is a concern in the community of adding toxicity by two drugs targeting EGFR in terms of more rash, diarrhea and gastrointestinal side effects, said Burns.
Patritumab deruxtecan, on the other hand, was associated with Grade 3 or higher events of thrombocytopenia, neutropenia and fatigue in 30%, 19% and 14% of patients respectively. In addition, drug-related interstitial lung disease (ILD) by central adjudication occurred in four patients, with one of them being Grade 3 or higher. ADCs as a class, especially the anti-Her2 ADCs, are associated with pneumonitis, said Halmos. The ILD associated with ADCs is less of a concern in breast cancer, but it is significant in NSCLC, said Griesinger. But based on available data, the risk with patritumab deruxtecan was manageable and not as high as other ADCs where it has been in the 10% range, said Halmos. Also, patients in the patritumab deruxtecan cohort were heavily treated, said Griesinger. Patients had received a median of four prior therapies. Management guidelines for suspected ILD include the administration of corticosteroids in particular situations, said the Daiichi spokesperson.
There will be toxicity tradeoffs with both approaches, and even if a drug causes lung toxicity it would be necessary to understand if that is manageable or if markers could help predict this, said Griesinger.
Manasi Vaidya is a Associate Editor for Clinical Trials Arena parent company GlobalData’s investigative journalism team. A version of this article originally appeared on the Insights module of GlobalData’s Pharmaceutical Intelligence Center. To access more articles like this, visit GlobalData.





Related Company Profiles
Johnson & Johnson
AstraZeneca Plc
Daiichi Sankyo Co Ltd