Researchers at Gladstone Institutes have developed a new method of making adult cardiac muscle cells (cardiomyocytes) in animal models divide and repair damage caused by heart attacks.
The study was led by Gladstone Institutes president Deepak Srivastava, with findings published in scientific journal Cell, and claims to be the first the first efficient and stable technique of its kind.
The investigation was inspired by the ability of organisms such as fish and salamanders to divide and regenerate tissue, repairing their own damaged or injured organs. While humans have this ability in embryonic form, following birth cardiomyocytes lose their ability to divide – as do other human cells such as those of the brain, spinal cord and pancreas.
“Because so many adult cells can’t divide, your body can’t replace cells that are lost, which causes disease,” Srivastava said. “If we could find a way to get these cells to divide again, we could regenerate a number of tissues.”
The researchers identified four genes involved in the process of cell division and found that when combined these genes cause mature cardiomyocytes to re-enter the cell cycle and allow cells to divide and reproduce rapidly.
“We discovered that when we increased the function of these four genes at the same time, the adult cells were able to start dividing again and regenerated heart tissue,” said the study’s first author Tamer Mohamed.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
By GlobalData“We also showed that, after heart failure, this combination of genes significantly improves cardiac function.”
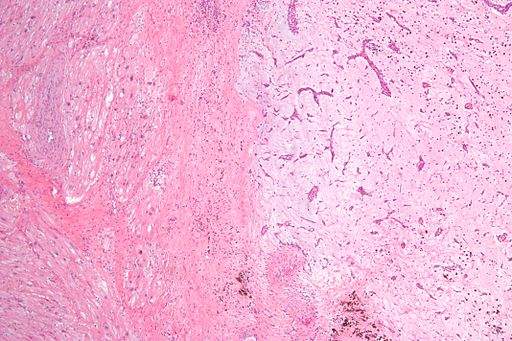
This newly-discovered method was then tested in animal models using cardiomyocytes derived from human stem cells. Newly-divided cells were genetically marked with a specific colour and monitored to discern whether the cells were truly dividing. Findings showed that the combination of the four genes caused 15-20% of the studied cardiomyocytes to divide and remain alive.
“This represents a considerable increase in efficiency and reliability when compared to previous studies that could only cause up to 1% of cells to divide,” said Srivastava.
“Of course, in human organs, the delivery of genes would have to be controlled carefully, since excessive or unwanted cell division could cause tumours.”
The researchers then examined ways of reducing the number of genes needed for the process to remain efficient. They found that the same results could be achieved by replacing two of the four genes with drug-like molecules.
More than 24 million people worldwide suffer from heart failure, with few available treatment options for late-stage patients other than a heart transplant. Over the years numerous studies have been set up attempting to activate cell regeneration, but until now these have been unsuccessful and poorly reproducible. Gladstone Institutes’ study offers new hope to those living with damaged hearts, offering the possibility of creating new heart tissue through cell division. As the genes used in their method do not occur only in the heart, the researchers have expressed their belief that the method could be used to divide and regenerate other types of adult cells.
“Heart cells were particularly challenging because when they exit the cell cycle after birth, their state is really locked down—which might explain why we don’t get heart tumours,” said Srivastava.
“Now that we know our method is successful with this difficult cell type, we think it could be used to unlock other cells’ potential to divide, including nerve cells, pancreatic cells, hair cells in the ear, and retinal cells.”
Such a development could mean finding regenerative treatment for brain damage, diabetes and loss of hearing and vision.
In recent years the field of regenerative medicine has received increasing levels of government support and public attention. For instance in Japan a series of reforms has accelerated the approval process for regenerative medicines, specifically due to the Pharmaceuticals and Medical Devices Act (PMD Act) and the Act on the Safety of Regenerative Medicine. These measures allow a route to commercialisation that is considered the fastest in the world.
At the beginning of March 2018, the California Institute for Regenerative Medicine (CIRM) board awarded $5.74 million to City of Hope to help fund a Phase I clinical trial examining a blood stem cell transplantation procedure for patients with severe sickle cell disease (SCD). If the trial shows positive results, City of Hope can extend it to treating autoimmune diseases such as type 1 diabetes.
In February 2018 a regenerative therapy initiative called Celularity was established in the US. The project involves a partnership between Singularity University founder Peter Diamandis and Celgene Cellular Therapeutics founder Robert Hariri. The initiative has already raised around $250 million and will examine placenta stem cells in the hope of finding new regenerative therapies.