In the medical device industry, there’s a constant struggle to develop new devices that are innovative, but cost-effective. The underlying problem is that there is a continuous pressure on the price setting of medical devices. As funds get tighter, there is less money to go around, which experts feel ultimately stifles innovation.
Some argue this is chiefly because the end user is not willing to pay the price. Even though companies can manufacture medical devices at a relatively cheap price, the regulatory process is so expensive that it deters companies from developing devices that are more groundbreaking.
This is an issue that has already been touched upon in recent times. For medical device companies, particularly start-ups, there is less money available to develop novel technologies. Finn Bjarke Christensen, CEO, FBC Device ApS, says this is not a device problem, but a societal problem as, ultimately, the patient suffers.
"We all need development in whatever we’re doing and we can’t get it for free and at the same time expect that development to go on," Christensen said.
What’s evident is a fight between reducing costs and developing new medical devices. Christensen says the industry has to play a fine balancing act. With less money to spend on resources, new and better technology is really suffering. While companies may be able to produce new devices at a cheaper price, producing something that is better is becoming a real challenge.
See Also:
To compound matters further, hospital sites are finding it more difficult to collect and conduct its own research. When placing fewer resources in the context of a lack of investment, it becomes apparent that the industry needs to be more supportive in providing the resources that could advance clinical studies.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
By GlobalData"I think the problem stems from the environment – it’s very money-driven, so you’ll find in some countries, there’s not enough support for clinical research, at least in Europe," said one medical device expert, who spoke on condition of anonymity.
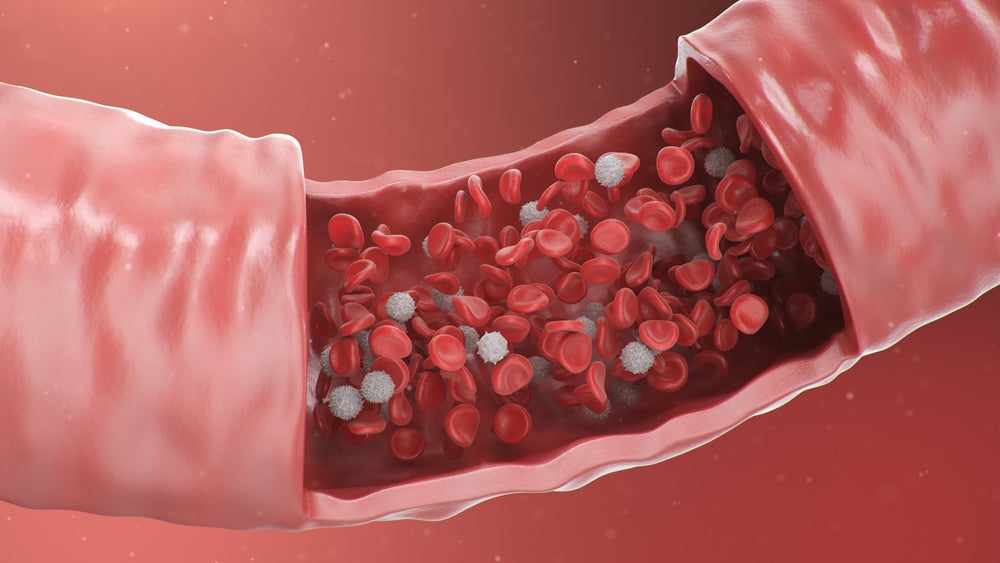
The medical device industry, the expert argues, is a commodity market. "If you look at cardiology, for example, every pacemaker and every implant is developed to a high technical standard, which is fine. But trial sponsors are investing a lot of money to protect their own interests. They don’t have the foresight to look left and right."
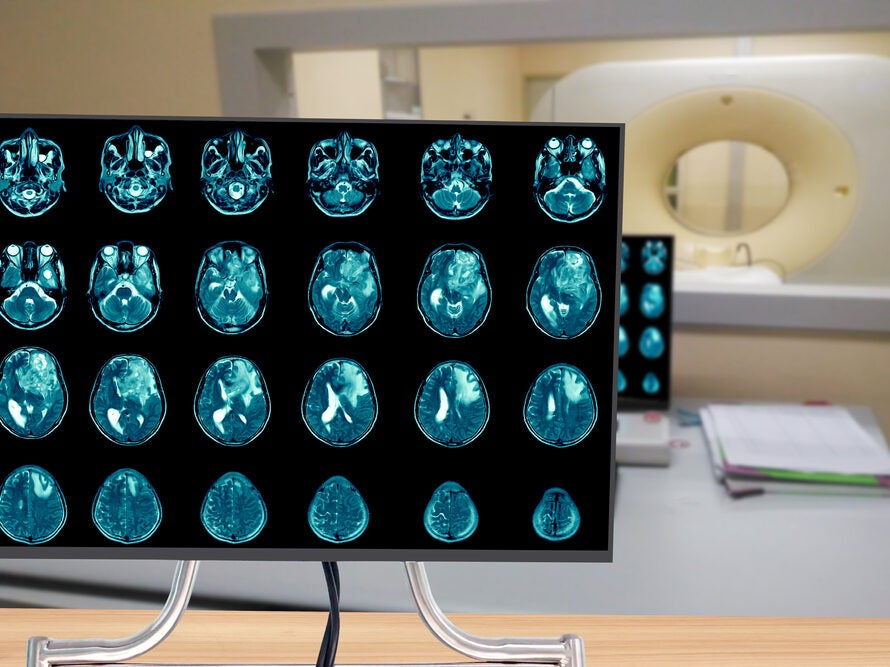
So it would appear there are no easy answers to resolve this problem. Furthermore, as technologies advance, medical devices are becoming more and more complex to handle and operate. That applies pressure on the site staff running the trial.
"For a young physician who just finished university starting a career in clinical research, it’s very hard to become an expert in this high-end technology," the expert said. "It requires you to have specialised knowledge of these devices."
Additionally, the pressure on sponsors to lower costs means manufacturers are reducing their technical services towards hospital sites. This means site staff aren’t being trained on how to use these new devices.
"While there’s lots of innovation out there, in some cases, the patients don’t benefit because hospital staff might not know how to use the devices properly," the expert said.
Another issue that the medical device industry faces is the fact that the device regulatory pathway is different in that there is no traditional phase I to IV approach in the design of a clinical trial.
"If you see the information from notified bodies on regulations of clinical trials, one glaring problem is the post-market clinical follow-up (PMCF) studies," said Christensen. "The problem is there aren’t any clear guidelines."
Christensen says it’s an area where regulatory bodies should answer the question: "’What are you concerned about?’ Then the sponsors should only make a protocol with the variables that analyse this specific area, and not try to fill out others the notified body claim they’re not worried about."
Christensen sees the PMCFs as an area where the industry can really affect the study design.
"You can save a lot of money, a lot of time, and reduce the number of patients needed to make reliable outcome statements."