At a time when commercial clinical trial patient recruitment has substantially declined in the UK, one borough completely bucked the trend recording a large increase.
During the Arena International Outsourcing in Clinical Trials UK and Ireland 2023 conference (OCT23) on 5 and 6 September, Dr Ian Bruce, director of the National Institute for Health and Care Research (NIHR) Manchester Biomedical Research Centre, discussed how Greater Manchester (GM) has seen a 44% increase in patients from 2017–18 to 2021–22. Meanwhile, the number of patients recruited over the same time frame nationally has dropped from more than 50,000 to 28,000, prompting a review into commercial clinical trials in the UK which was conducted by former health minister Lord James O’Shaughnessy.
O’Shaughnessy says that the review has provided practical recommendations after speaking to a variety of specialists in the industry, including those in Greater Manchester. “We need to rejuvenate the whole industry so you’ve got to be honest about some of the problems we’re facing, such as slow setup times,” O’Shaughnessy says. “The review is all about giving practical recommendations to the government and all the other actors who need to make stuff happen like the NHS, to make a difference in the short term.”
The Greater Manchester model
In what has been coined the Greater Manchester model, the borough also boasts quicker start-up times for clinical trials at an average of 51 days compared to the national average of 117 days. Another area in which Greater Manchester is ahead is that while 60% of trials deliver to time and target on average across England, Greater Manchester has consistently exceeded the target of 80% for the last decade.
Speaking directly to the Clinical Trials Arena team, Bruce says that the key to success for the borough following the pandemic has been a result of a combination of factors including having a good relationship with the patient population, strong research infrastructure and a talented workforce, collaboration between providers, academia and industry, and a supportive business environment.
“If you organise well and you have a good relationship with the population, you can recover and get more trials back up and running again,” Bruce explains. “This is combined with our shorter approval times which means that companies are also happy with what we're doing. We have long-term strategic relationships with CROs and companies where we're the prime site for recruitment. They're pleased with our performance and they want to send more studies our way.”

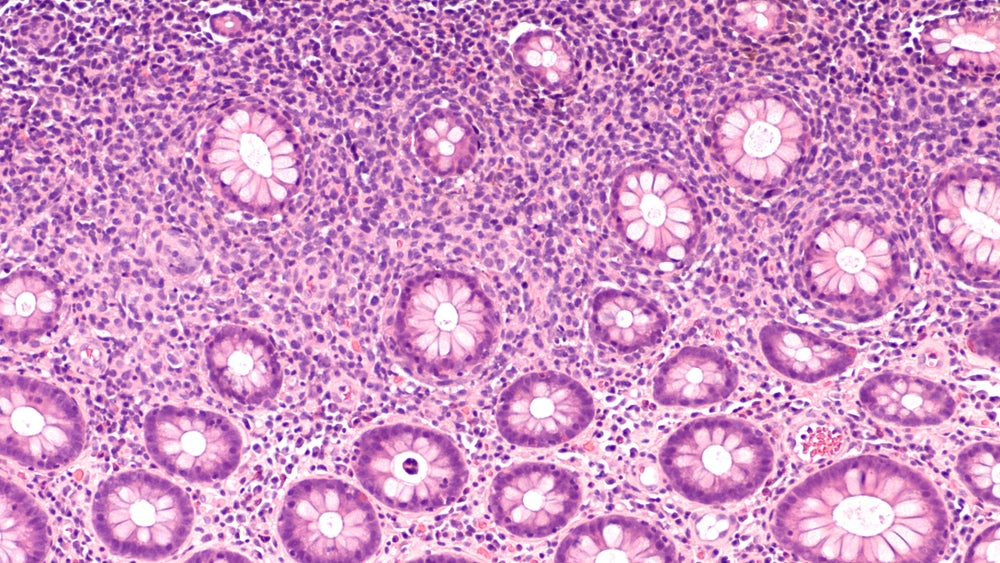
Due to previously recorded success in clinical research, Manchester received Academic Health Science Centre (AHSC) designation in 2020 by NIHR, NHS England and NHS Improvement until 2025. The Manchester AHSC brings together the University of Manchester, Manchester University NHS Foundation Trust (MFT), The Christie NHS Foundation Trust, Salford Royal NHS Foundation Trust (part of the Northern Care Alliance NHS Group) and Greater Manchester Mental Health NHS Foundation Trust (GMMH). The MAHSC will lead across six therapy areas including cancer, cardiovascular and diabetes, inflammation and repair, mental health, neuroscience, and women and children.
Patients should be at the heart of trial design
Bruce also highlighted the importance of bringing research to patients as the borough focuses on conducting trials that are of relevance to the community.
“We did some heat maps of where patients who were being recruited to studies in Manchester came from and a disproportionate number were coming from the nicer suburbs of Manchester,” Bruce says. “We realised that the patient populations weren't as representative as they could be so we've made deliberate moves now to recruit patients from a wider spectrum of populations.” Another way Bruce said to engage patients is to ensure they are involved in designing the research they will be a part of. “You want your public to understand why medical research is important and how it can help shape lives and improve outcomes,” Bruce explains. “We spend a lot of time getting the patients involved in the design of our studies, prioritising what we should look at and then we are prioritising the way in which we study these areas. We really want to embed the patient's voice into the studies so that they're being more involved, they trust researchers better and are more likely to participate in studies and trials.”

One example Bruce cited was when a colleague was conducting a study about brain fog in patients with lupus. The researchers questioned patients about when they needed breaks and the order in which they would like to complete the tests to ensure the study design was personalised for them. As a result, more patients returned for later stages of the trial.
Replication requires regions making the most of their infrastructure
Other areas of the country are now looking to replicate the model to improve commercial clinical trial initiation across the country. The main way to do this is to ensure collaboration across the board.
Speaking at a panel at OCT23, Dr Janet Messer, director of approvals service at the Health Research Authority (HRA) said that it is good to see collaboration as opposed to competition in Greater Manchester. “A lot of what has been achieved in Manchester is because organisations have collaborated instead of competing with each other,” Messer says. “Historically, in the UK, we have tended to have systems where NHS organisations have always been pitted against each other. And so they start gaining things, they are trying to get to the top of the league and they're not actually focused on the real prize, which is delivery of good research and making sure that researchers make trials available to patients, and that they're really supporting both commercial and non-commercial research. And I think that shift has absolutely happened in recent times with examples like Manchester.”

In the same panel chat, Alison McMorn, vice president of clinical development at AMO Pharma says it is good to know that efficient research is being conducted in the UK. “I think the example of Manchester and what has been done in the North West is incredible,” McMorn says. “It's really heartening and it shows that good, efficient research can be done and that it's not a complete downer for the UK.
O’Shaughnessy echoes the calls that collaboration needs to be at the top of the list for the UK to be successful in commercial trials. “If we are to rejuvenate the commercial clinical trial sector we need to listen to the customer and the customer is industry,” O’Shaughnessy explains. “Of course, they will have various demands, but they also have lots of expertise. And so, co-producing these reforms is going to be really important.”
Bruce says that a vital step for Greater Manchester improving patient outcomes is ensuring it has a robust clinical trial infrastructure. “Our focus is on improving health outcomes in our patients and our population as quickly as possible and we want to accelerate those outcomes and improvements. Clinical trials is one of the steps in that. If you've got that focus of accelerating improvement for your patients and your citizens then you have to coordinate your clinical trials better.”
Areas with large infrastructure will be able to replicate the Greater Manchester model with relative ease; the difficulty will come for regions where they do not have the same access to facilities. Bruce explains that to overcome this is to utilise what infrastructure there is in the region and build it up.
“It’s the idea of integrating and coordinating your infrastructure. It doesn't just have to be large conurbations that do that. If you've got several district general hospitals and a primary care base that's interested in research, coordinating people at that level, as long as everybody understands what they are doing and align their aims and objectives, they should succeed.”