At IDWeek 2025, (the joint annual meeting of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, the Pediatric Infectious Diseases Society and the Society of Infectious Diseases Pharmacists) held from 19 to 21 October in Atlanta, Georgia, Dr Camille Kotton from Massachusetts General Hospital, Boston, presented data from a Phase II clinical trial assessing the efficacy and safety of pritelivir versus foscarnet for the treatment of acyclovir-refractory and/or resistant mucocutaneous herpes simplex virus (HSV) infections in immunocompromised patients.
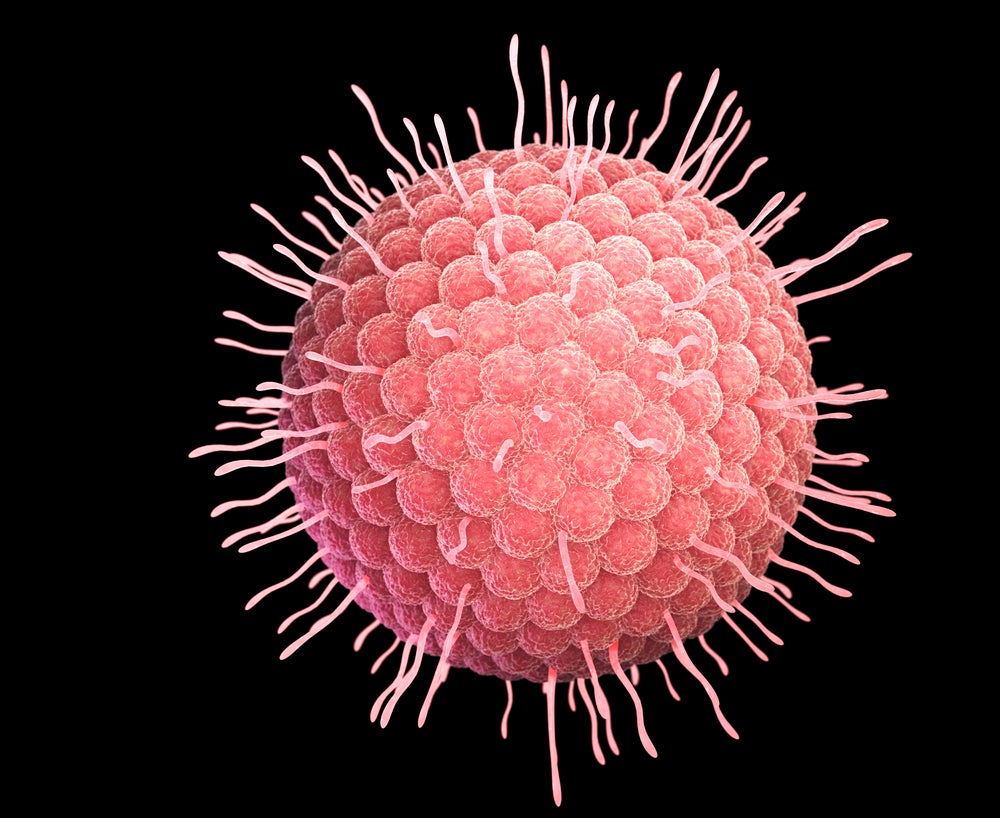
HSV is a virus of the herpesviridae family. There are two types of HSV: HSV-1 is predominately an orally transmitted infection and causes cold sores around the mouth, and HSV-2 is a sexually transmitted infection (STI) and predominately causes genital herpes. Co-infection with both HSV-1 and HSV-2 can also occur. HSV infections are not curable, but antivirals can be used to manage symptoms.
The management of HSV infections among immunocompromised patient populations can be particularly challenging as these patients are more prone to severe, prolonged and refractory HSV infections that do not respond to standard-of-care antivirals such as acyclovir, valacyclovir and famciclovir. The resulting painful lesions can have a severe impact on quality of life and lead to severe and potentially fatal complications such as encephalitis, pneumonitis and hepatitis. Due to improved cancer treatments and other medical advances, the proportion of the global population that is immunocompromised has increased substantially in recent years, making this a growing problem.
Refractory HSV is defined as a lack of clinical improvement in HSV-positive lesions after at least seven days of appropriately dosed antiviral therapy, or the appearance of new HSV-positive lesions after receiving appropriately dosed antiviral therapy for at least seven days. Resistant HSV is a subset of refractory HSV associated with one or more viral genetic alterations that decrease susceptibility and/or phenotypic assay demonstrating increased half-maximal inhibitory concentration (IC50) above the assay cutoff to one or more antiviral therapies.
Foscarnet, an antiviral in use since the 1990s, is currently the mainstay of treatment for refractory and resistant HSV infections. However, the therapy has considerable limitations. It is associated with clinical improvement in only about half of this patient population. It is also considerably nephrotoxic [damaging to the kidneys] and requires intravenous administration.
Aicuris’s pritelivir is a small molecule with a novel mechanism of action and strong potential to address some of these limitations. The US Food and Drugs Administration has granted pritelivir breakthrough therapy designation and it has demonstrated activity against nucleoside analogue and foscarnet-resistant HSV-1 and HSV-2 isolates in vitro. It is orally bioavailable with a half-life of 60 days, allowing for once-daily dosing. Additionally, studies demonstrate that pritelivir does not exhibit clinically relevant drug-drug interactions.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe PRIOH-1 Phase II trial recruited immunocompromised adults, including those living with HIV, haematopoietic cell transplant recipients, solid organ transplant recipients and those with chronic glucocorticoid use, who had clinical failure, refractory disease and/or positive genotypic/phenotypic resistance testing. In Part A of the trial, patients were randomised to receive treatment with either pritelivir or foscarnet. A total of 14 out of 15 treated patients (93.3%; confidence interval (CI) 95%, 68.1–99.8) achieved healed lesions in the pritelivir arm compared to four out of seven treated patients (57.1%; CI 95%, 18.4–90.1) in the foscarnet arm. This equated to a treatment difference of 36.2% (CI 95%, 10.1–74.1).
Part B of the trial involved a non-randomised single arm of pritelivir in a more heavily treatment-refractory population. Patients were acyclovir or foscarnet-refractory/resistant or foscarnet-intolerant based on clinical failure/refractory disease and/or prior cessation of foscarnet therapy and/or positive genotypic/phenotypic resistance testing. In Part B, five out of eight pritelivir-treated patients (62.5%; CI 95%, 24.5–91.5) achieved healed lesions.
The safety and tolerability data for pritelivir was also favourable. Two out of 23 pritelivir-treated patients (8.7%) in the study experienced drug-related treatment emergent adverse events, compared to five out of seven foscarnet-treated patients (71.4%).
The data from the PRIOH-1 Phase II trial are highly encouraging. Although the study was small, pritelivir clearly demonstrated numerically improved efficacy relative to foscarnet, as well as a more favourable safety and tolerability profile. A Phase III pivotal trial in refractory HSV-infected immunocompromised patients is currently underway, with initial results indicating that pritelivir met the primary endpoint, achieving highly statistically significant superiority over standard-of-care therapies. Topline data are anticipated in early 2026.
Aicuris has announced that it is preparing to submit a new drug application to the FDA in 2026. The company is highly likely to attain regulatory approval for its lead candidate. With the potential to provide the HSV-infected immunocompromised population with safer, more convenient and more effective means to manage symptoms, pritelivir is expected to be a game changer, resulting in substantial quality-of-life improvements for patients. Additionally, as the percentage of the global population that is immunocompromised continues to increase in the coming years, Aicuris anticipates an expanding target patient population.