The European Medicines Agency estimates that up to 40 clinical trials of stem cell therapies are currently underway within the European Union alone, with many more being conducted in other parts of the world.
Below is a list of several recent developments.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Spinal cord injuries
The US Food and Drug Administration (FDA) has recently approved a Phase I clinical trial of a stem cell-based treatment for acute spinal cord injuries. Geron’s GRNOPC1 drug contains human embryonic stem cells-derived oligodendrocyte progenitor cells, which have demonstrated remyelinating and nerve growth stimulant properties in animals with spinal cord injuries.
Administered seven days after the incident, the treatment replenishes oligodendrocytes, which are lost in spinal cord injuries. Oligodendrocytes produce myelin and neurons, the absence of which causes paralysis in spinal cord injury victims.
Patients with complete American Spinal Injury Association Impairment Scale grade A subacute thoracic spinal cord injuries will take part in the trials, which assess the drug’s safety and efficacy.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataGeron suffered a setback during preclinical expansion studies when a higher frequency of animals developed cysts in the injury site than had been seen in previous studies. As a result, GRNOPC1 was optimised to develop new candidate markers and assays, and the FDA allowed clinical trials to commence in July 2010.
In addition to spinal cord injuries, GRNOPC1 may have therapeutic benefits for other central nervous system complications, including Alzheimer’s disease, Canavan disease and multiple sclerosis, with collaborations already underway to test the medication in animal models.
Stroke rehabilitation
In February this year, the UK Gene Therapy Advisory Committee (GTAC) allowed the UK-based ReNeuron to launch Phase I clinical trials of its ReN001 stem cell therapy, designed to help patients left disabled by an ischaemic stroke, the most common form of the condition.
ReNeuron CEO Michael Hunt said the final approval would pave the way for subsequent cell therapy applications.
Intended for patients in the post-stroke rehabilitation phase, ReN001 aims to improve both functional and cognitive recovery.
There are currently no therapies available for patients who have a stable and fixed neurological deficit following a stroke, but ReNeuron hopes this can be addressed with ReN001.
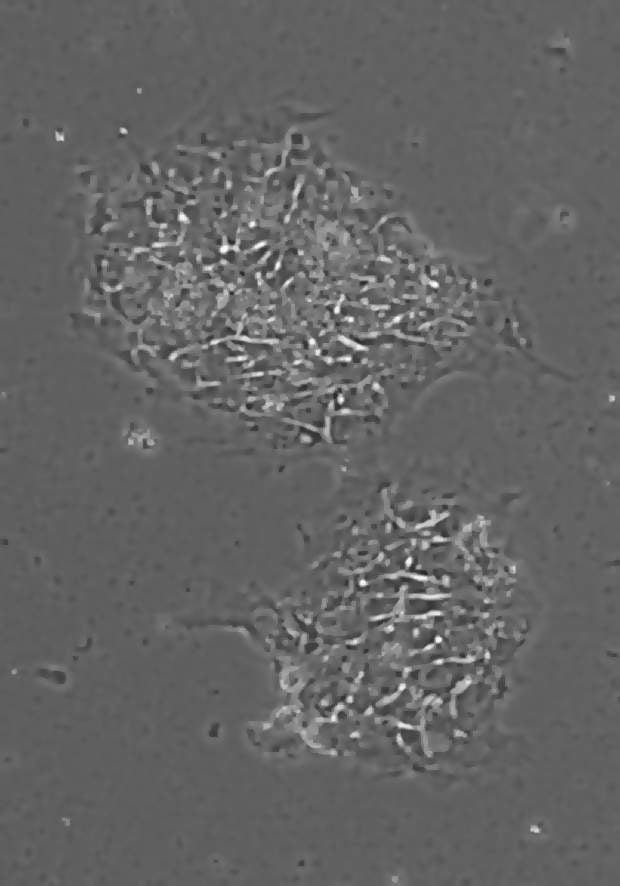
Consisting of a neural cell line called CTX, generated using ReNeuron’s proprietary cell expansion technologies, ReN001 has been shown in pre-clinical testing to reverse the functional deficits typically associated with stroke disability when administered several weeks after the event.
Patient recruitment has already commenced in the UK for Phase I clinical trials, which will evaluate the safety of the implantation technique, establish the side-effect profiles associated with the therapy, and collect preliminary efficacy data.
Treating cancer
Stem cells have long been considered a prospective treatment for cancer patients, and Bayer Schering and OncoMed announced in June a strategic alliance to attempt to develop antibodies, protein therapeutics and small molecules to target the Wnt signalling pathway, which determines the establishment, metastasis and recurrence of cancer stem cells.
Recent studies have shown that adult stem cells administered both intravenously and subcutaneously reduced cancer size and increased life span in canines with tumours. Human stem cells were also administered to a group of mice previously infused with melanoma, with similarly positive results in cancer size and lifespan.
These results followed research conducted at the Harvard Medical School, where human neural stem cells were transplanted into the brains of rodents with intracranial tumours. Within days, the cells migrated towards the cancerous area and produced the enzyme cytosine deaminase, capable of converting non-toxic pro-drugs into chemotherapeutic agents.
This resulted in an 81% reduction in tumour mass, and the stem cells neither differentiated nor turned tumorigenic, leading researchers to believe that stem cell-based therapies could treat cancer and distinguish between cancerous and non-cancerous cells.
Type 1 diabetes
Stem cell treatments have been shown to significantly reduce type 1 diabetes sufferer’s dependence on insulin, allowing them to go, on average, almost two and a half years without using multiple daily injections to manage the condition.
The treatments works by ‘resetting’ the immune system, causing it to no longer attack the pancreas, the organ responsible for producing natural insulin. The treatment must be used as early possible, usually within six weeks of diagnosis, before irreparable damage has been done to the pancreas or complications relating to high blood sugar levels have set in.
The research was initially conducted by Dr Carlos EB Couri and colleagues from the University of Sao Paulo, Brazil, in partnership with Dr Richard K Burt from the Division of Immunotherapy, Northwestern University Feinberg School of Medicine, Chicago.
A total of 23 individuals were treated with autologous nonmyeloablative hematopoietic stem cell transplantation (HSCT) with stem cells derived from bone marrow, a process more commonly used to treat leukemia. Stem cells were then extracted and released. Subjects were also given a course of cytotoxic conditioning drugs to partly suppress the response of the patient’s immune system.
In all, 20 of the 23 individuals tested during the programme remained free from insulin injections, with 12 staying insulin-free for an average of 31 months and eight relapsing to a small daily dosage of insulin. The researchers concluded the treatment "remains the only one capable of reversing type 1 [diabetes mellitus] in humans".
Alongside the treatments outlined above, there have also been moves to treat various other illnesses using stem-cell inspired therapies, including deafness, blindness, amyotrophic lateral sclerosis and even infertility.





