An affordable hepatitis C combination therapy has been demonstrated to be a safe and effective treatment, with interim results from the Phase II/III STORM-C-1 trial reporting high cure rates for patients.
The combination treatment consists of sofosbuvir and ravidasvir, medications made by Egyptian drug manufacturer Pharco Pharmaceuticals.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
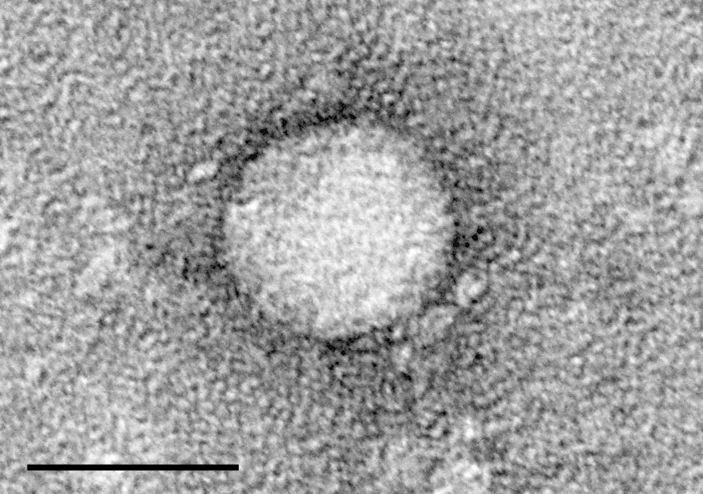
Ravidasvir is a new oral inhibitor of NS5A, while sofosbuvir is an inhibitor of the NS5B polymerase, viral proteins found in the hepatitis C virus (HCV). Both have been demonstrated to have high potency, low side effects and a high barrier to resistance.
Agreements signed in 2016 and 2017 set a target price for the combination at $300 for a treatment course of 12 weeks, (equating to $3.50 per day), a far cheaper alternative to other HCV treatments available, many of which cost thousands of dollars. For instance, Gilead’s blockbuster hepatitis C treatment Sovaldi (sofosbuvir) launched in the US at a price of $84,000 per course, although lower prices have been negotiated elsewhere.
The results were presented at the International Liver Conference in Paris by the non-profit organisation Drugs for Neglected Diseases initiative (DNDi), which conducted the trial. The study was co-sponsored by the Malaysian Ministry of Health and took place across ten sites in Malaysia and Thailand.
“The…combination is comparable to the very best hepatitis C therapies available today but it is priced affordably and could allow an alternative option in countries excluded from pharmaceutical company access programs,” DNDi executive director Bernard Pécoul said.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataDNDi conducted the trial to evaluate the efficacy, safety and tolerability of the ravidasvir/sofosbuvir treatment. A total of 301 patients were given the combination treatment; those without cirrhosis of the liver were trialled over a course of 12 weeks, while those with compensated cirrhosis were trialled for 24 weeks.
After a 12- week period following treatment completion, 97% of participants were cured, measured using international standards defining cure for HCV treatments. Even those with the hardest- to- cure forms of the disease reported high cure rates. These included patients with liver cirrhosis at 96%, patients with HIV at 97%, those infected with genotype 3 at 97%, and those who had been exposed to previous HCV treatments at 96%.
Even patients with several of these risk factors were cured, with no unexpected safety signals detected.
Further trials are planned, with the aim of evaluating the efficacy and safety of the combination in patients infected with other HCV genotypes.
“From a treatment provider perspective, this is very exciting as we have been waiting for a simple, affordable, robust treatment tolerated by all patients groups, including those whose treatment outcomes are currently poorer, like patients under antiretroviral therapy,” deputy operations director for Médecins Sans Frontières / Doctors Without Borders (MSF) Pierre Mendiharat said.
“This will be crucial to expand treatment to the most vulnerable categories of patients in developing countries.”
MSF has been collaborating with DNDi to help increase accessibility to treatment for HCV patients in low- and middle- income countries, with the STORM-C project financed by MSF’s Transformational Investment Capacity (TIC) initiative.
The Malaysian government has also been working to improve treatment options for those living with the condition. A ‘government-use’ licence on sofosbuvir was issued in September 2017, enabling 400,000 people living with hepatitis C in Malaysia to access generic HCV regimens in public hospitals.
“As hepatitis C has become a major public health concern in Malaysia, it is crucial to increase access to treatment for the benefit of the nation,” Malaysian director general of health Dr Datuk Noor Hisham Abdullah said.
Worldwide over 71 million people live with hepatitis C, a blood-borne infection that can cause liver cirrhosis, cancer and death. The UK has an estimated 215,000 HCV cases, while the US has 3.4 million. Around 400,000 HCV-related deaths are reported each year.
Though effective medications exist, less than three million people are on treatment and more people are diagnosed with the condition every year than are put on treatment.
Gilead has lowered the cost of its HCV treatment Harvoni, though its $48,000 price-tag for a 12 week treatment course means it is still too expensive to allow its use in large-scale treatment programmes.
Similarly, AbbVie launched its HCV drug, Mavyret, last year with an eight-week treatment cost of $26,400.
The World Health Organisation (WHO) has said it aims for 80% of patients diagnosed with HCV to be put on treatment by 2030, an aim that has thus far seemed unattainable due to the high price of medication.





