Researchers at UC Davis Health and Albany Medical College in the US have identified the protein vascular endothelial growth factor A (VEGFA) as a potential new target for asthma treatments.
The study, published in the Journal of Allergy and Clinical Immunology, demonstrated the role of group 2 innate lymphoid cells (ILC2s) in airway hyperresponsiveness (AHR), with VEGFA as one of the highest expressed genes in activated ILC2.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Previously VEGFA was known for its stimulation of tumour growth, however the latest findings highlight its role in the inflammation and airway obstruction associated with asthma.
A team led by UC Davis respiratory immunologist Dr Angela Haczku, in a previous collaboration with Albany Medical College immunology professor Dr Qi Yang, found that ILC2s can help to stimulate AHR. This is when an asthma attack is triggered by the lungs responding to allergens or toxic air pollutants such as ozone.
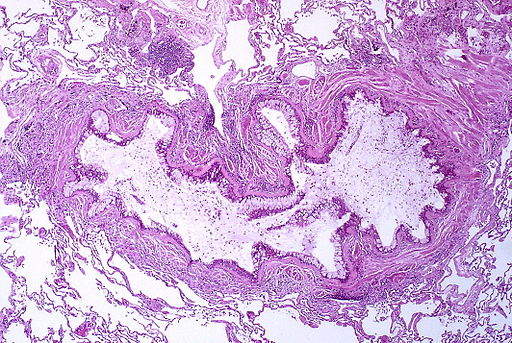
“These ILCs produce an influx of inflammatory neutrophils into the lungs, and we do not know exactly what mediates this cellular inflammation,” Yang said. “These cells are very important in many diseases, including infections and pollutant-induced lung injury, which could be mediated by the inflammatory cells in the lungs.”
Following the discovery the team focused its investigation on the types of inflammatory molecules produced by ILC2s, which activate the inflammation.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“We couldn’t figure out what was actually causing the airway obstruction,” Haczku said. “How do these innate lymphoid cells cause asthma?”
The researchers examined reactions in mouse models to the common allergen Alternaria alternata. Inflammation was observed within the first few hours, however after VEGFA inhibitor SU1498 was administered the inflammation and immune response reduced. A further study demonstrated the efficacy of inflammatory immune molecule interleukin-33 to stimulate ILC2s, with SU1498 also effectively targeting the molecule.
“VEGFA was very strongly upregulated in asthma patients and animals that receive stimulations that cause asthma,” said Haczku. “This mediator can actually elicit the symptoms of asthma in the mouse model and, if you target it, you eliminate the asthma symptoms.”
Asthma treatments have generally consisted of glucocorticoid inhalers, though more recently monoclonal antibodies have been favoured for their ability to target molecules with more precision.
“Monoclonal antibodies can target very specific molecules rather than knocking out the entire immune system,” Haczku said. “Some of these antibodies target cytokines that also mediate allergic symptoms and asthma. We hope that targeting VEGFA, or the VEGFA receptor, with such monoclonal antibodies would add to this armamentarium.”
The researchers aim to continue examining ILC2s, investigating their potential role in other lung conditions.





