Verigraft has enrolled half of the planned 15 patients for its first-in-man trial investigating the safety and efficacy of its personalised tissue-engineered veins (P-TEV), Verigraft CEO Petter Björquist told Medical Device Network.
Two patients have reached the 12-month endpoints of the trial, which Björquist says will complete enrolment in June 2024.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The trial’s primary endpoints are safety orientated such as the risk of infection, mechanical failure and rejection rate while the secondary endpoints will assess efficacy.
The trial is investigating Verigraft’s technology in patients with chronic venous insufficiency, where faulty valves do not prevent backflow of venous blood. This results in increased hydrostatic pressure in the lower leg.
Swedish-based Verigraft’s spearhead vein product uses the company’s cellular technology which personalises tissue to improve transplant acceptance. Björquist explains that by tailoring tissue to the patient using their own cells, the need for excessive immunosuppression is not needed.
Patients undergoing transplants usually take immunosuppressive agents to reduce the chance that their body rejects the new tissue, but this makes them susceptible to other diseases.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
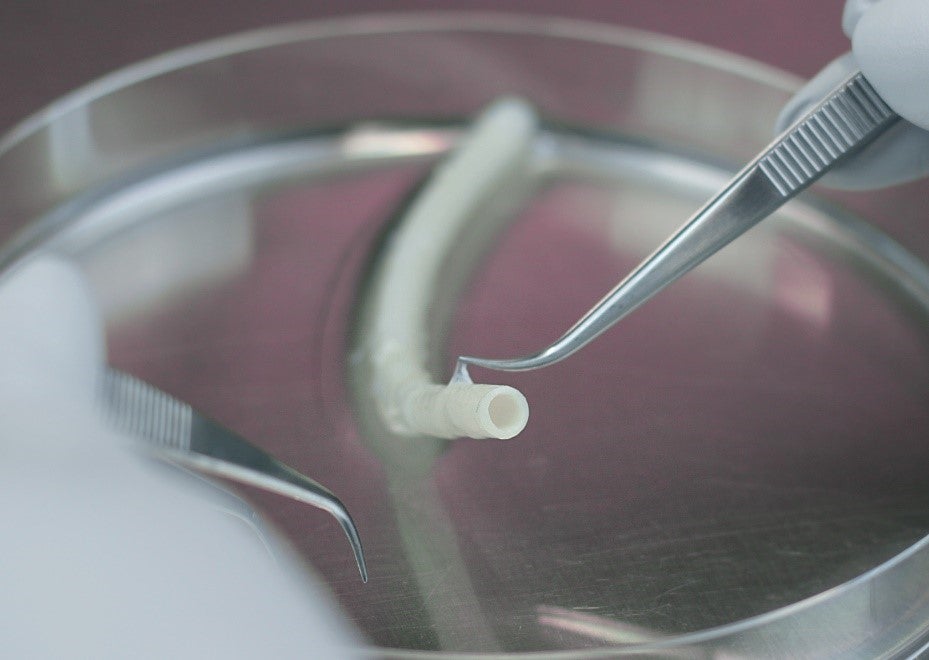
By GlobalDataThough personalised tissue is not new, Björquist says that the technique Verigraft uses to isolate patient cells – which it adds to a decellularised scaffold of tissue from a donor – takes around ten days. Currently, cell isolation processes can take around six months. Björquist adds that the donor scaffolds can be put aside and used further down the line – Verigraft has tested ones stored for more than a year.
Though Verigraft is prioritising the venous market, Björquist unveiled plans for targeting the artery transplant market. Most of the latter market is dominated by synthetic graphs, Björquist explains that, despite their availability, biological graphs offer distinct advantages. Verigraft will also explore 3D-bioprinted grafts within the decade to produce a steady supply of scaffolds.
Speaking on plans around regulatory applications, Björquist said: “When discussing this with European and American authorities, we have concluded that some 82-100 patients should be enough to have data.”
GlobalData medical analyst Ashley Clarke said in a viewpoint from April 2023: “Tissue-engineered skin substitutes (TESSs) have widespread uses in wound care for treating skin defects and injuries and are advantageous for use in serious or chronic injury where the skin’s natural ability to heal may be disrupted.
“According to GlobalData, a leading data and analytics company, sales of TESSs are expected to grow to $3bn by 2033 from $2bn in 2023, with acellular skin substitutes composing 62% of the market. GlobalData attributes this market growth to the increasing prevalence of injuries and chronic diseases globally, as well as higher adoption of technologically advanced healthcare practices like regenerative and personalised medicine.”





