Cablivi™ (caplacizumab) is a bivalent anti-Von Willebrand factor (vWF) nanobody indicated for the treatment of adults with acquired thrombotic thrombocytopenic purpura (aTTP).
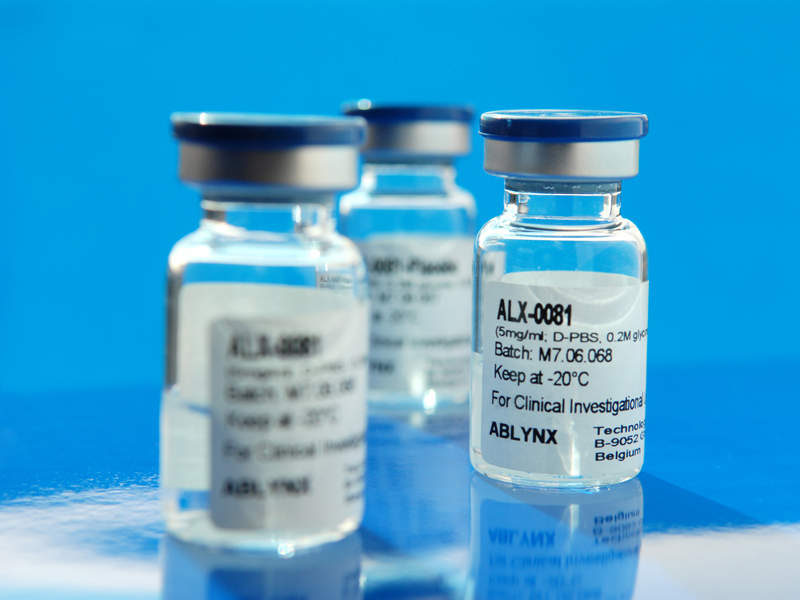
One of the first therapeutics to have received approval for the treatment of aTTP, the drug was initially developed by Belgium-based biopharmaceutical company Ablynx. French pharmaceutical company Sanofi acquired Ablynx for approximately €3.9bn ($4.57bn) in January 2018, adding Cablivi to its pipeline.
Cablivi received orphan drug designation in the US and Europe in 2009. Ablynx submitted a marketing authorisation application (MAA) for the drug to the European Medicines Agency (EMA) in February 2017.
The Committee for Medicinal Products for Human Use (CHMP) gave a positive opinion for granting marketing authorisation (MA) to Cablivi in June 2018. The European Commission (EC) also granted MA in September of the same year.
Cablivi has also received fast track designation from the US Food and Drug Administration (FDA) for the treatment of aTTP. Ablynx submitted a biologics license application (BLA) for the drug to the FDA in the first half of 2018.
The FDA accepted the application and gave priority review status in September 2018. The drug received FDA approval in February 2019.
Thrombotic thrombocytopenic purpura symptoms and causes
Thrombotic thrombocytopenic purpura (TTP) is a rare autoimmune blood clotting disorder caused by lack of activity in the ADAMTS13 enzyme.
TTP is divided into inherited thrombotic thrombocytopenic purpura (iTTP) and aTTP. iTTP is passed genetically and is characterised by an abnormal ADAMTS13 gene, which causes inadequate ADAMTS13 enzyme production in the body.
aTTP is caused by certain antibodies hindering the ADAMTS13 enzyme. As a result, ultra-large Von Willebrand factor (ULvWF) molecules remain uncleaved due to the impaired ADAMTS13 enzyme.
vWF plays a crucial role in the platelet adhesion stage of blood clotting. The uncleaved ULvWF binds to blood platelets causing blood clots throughout the body.
The condition is life-threatening and leads to low platelet count, lack of blood supply to tissues (ischemia) and organ damage. Common symptoms of the disease include purple bruises or dots on the skin, fatigue, fever, paleness of the skin, increased heart rate, headache, coma and seizure. Around 95% of all TTP cases are aTTP.
Cablivi’s mechanism of action
The caplacizumab contained in Cablivi targets the vWF protein in the blood, blocks the interaction of ULvWF with platelets and inhibits platelet adhesion.
Cablivi is available as a 10mg powder or solvent for intravenous or subcutaneous injection.
Clinical trials on Cablivi
The EMA’s approval of Cablivi was based on the positive results of a Phase II clinical trial named TITAN and a Phase III trial called HERCULES, conducted on 220 adult patients with aTTP.
The HERCULES clinical trial was a randomised, double-blind, placebo-controlled, multi-national study with time-to-platelet count response as the primary endpoint. A total of 145 patients were randomised to receive either Cablivi or placebo.
Cablivi met the primary endpoint and demonstrated a statistically significant reduction in time-to-platelet count response. Reduction in aTTP-related death, recurrence or at least one major thromboembolic event was observed in approximately 74% of patients in the Cablivi arm, while a reduction in aTTP recurrence was demonstrated in 67% of patients.
TITAN was a single-blind, randomised, placebo-controlled trial that enrolled 75 adult patients that were randomised to receive either Cablivi or placebo. Patients receiving Cablivi showed a significant reduction in time-to-platelet count response when compared with placebo.
The FDA’s approval of the drug was based on the results of the HERCULES clinical trial.
The most common adverse events reported in patients during the trial were nosebleeds, headaches and bleeding gums.