Elzonris™ (tagraxofusp-erzs) is an interleukin-3 receptor alpha chain (CD123) directed cytotoxin that is indicated for the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN) in adults and paediatric patients.
Developed by US-based commercial-stage biopharmaceutical developer Stemline Therapeutics, the drug is recommended for patients that are at least two year’s old.
Stemline Therapeutics submitted a biologics license application (BLA) for the drug to the US Food and Drug Administration (FDA) in June 2018. The application was accepted and granted priority review status in August of the same year.
The FDA approved the drug as a treatment for BPDCN and gave breakthrough therapy and orphan drug designations in December 2018.
Stemline obtained accelerated assessment status for the drug from the European Medicines Agency (EMA) in November 2018 and submitted a marketing authorisation application (MAA) in January 2019.
The drug is also being evaluated for the treatment of chronic myelomonocytic leukaemia (CMML), myelofibrosis and other CD123-positive indications.
Blastic plasmacytoid dendritic cell neoplasm causes and symptoms
BPDCN is an aggressive blood cancer that is characterised by the overexpression of CD123 in tumour cells.
It primarily affects the blood, bone marrow, lymph nodes, spleen and skin. It is characterised by the malignant proliferation of cells originating from the plasmacytoid dendritic cell (pDC) precursor. These pDCs are produced in the bone marrow, circulate in the blood and accumulate in the lymph nodes due to an abnormal immune response.
BPDCN can occur at any age, but the median age at diagnosis is between 60 and 70 years. The disease is often misdiagnosed as non-Hodgkin lymphoma (NHL), acute myeloid leukaemia (AML), leukaemia cutis, melanoma and lupus erythematosus and has shown poor outcomes in patients. It is diagnosed based on the immunophenotypic diagnostic triad of CD123, CD4 and CD56.
Some of the common symptoms of the disease include lesions on the skin, rashes or bruise-like macules, anaemia and neutropenia, as well as a low red and white blood cell and platelet count.
Elzonris mechanism of action
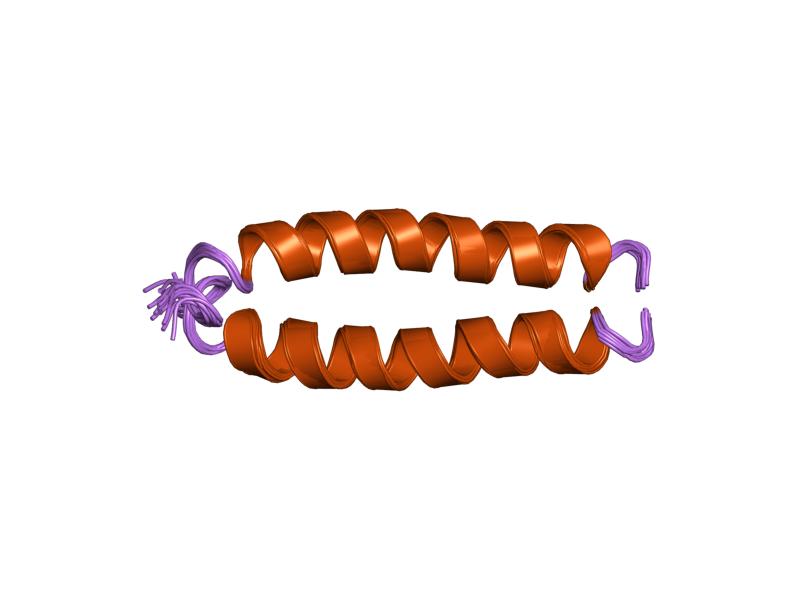
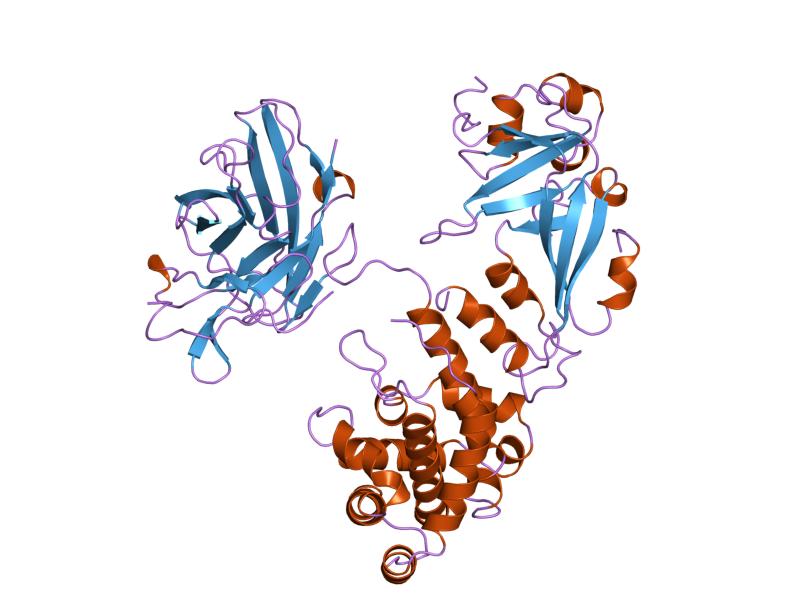
Elzonris is a novel targeted therapy directed to CD123 of the tumour cells. It is composed of truncated diphtheria toxin (DT) fusion protein and recombinant human IL-3.
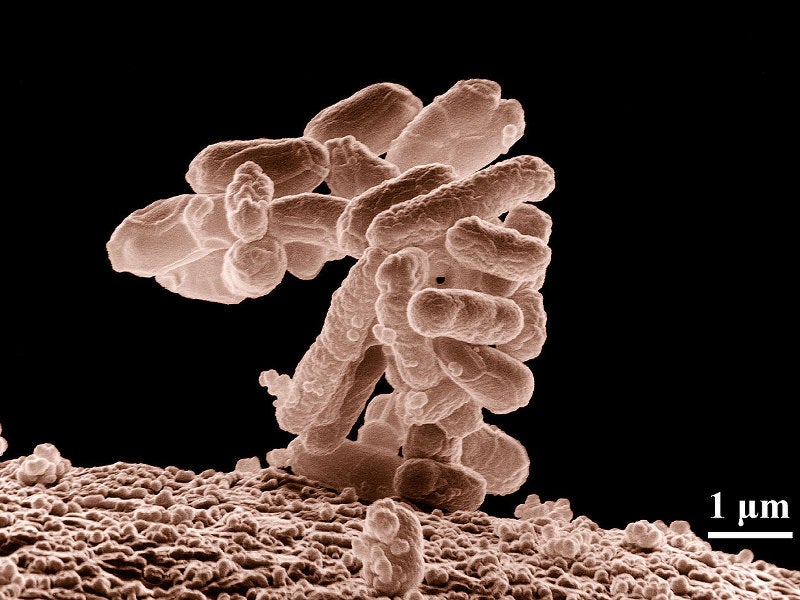
The IL-3 binds to the CD123-expressing tumour cells and delivers the cytotoxic diphtheria toxin to the cells, resulting in the blockage of protein synthesis in the cell and causing cell death. The drug is developed by recombinant DNA technology and produced in Escherichia coli cells.
Elzonris is available as a 1,000mcg/ml preservative-free, sterile, colourless solution in single dose vials for intravenous administration.
Clinical Studies on Elzonris
The FDA’s approval of Elzonris was based on the positive results of two multi-centre, open-label, single-arm clinical trials named STML-401-0114 and STML-401-0114, which were performed in two groups of patients.
In the first group, 13 previously-untreated BPDCN patients were enrolled and administered with 12mcg/kg Elzonris once-daily in the first five days of a 21-day cycle. The drug was administered through infusion syringe pump over 15 minutes.
The rate of complete response or clinical complete response (CR/CRc) was the primary endpoint of the trial. The primary endpoint was reached by approximately 54% of the patients.
The second group comprised 15 patients with relapsed or refractory BPDCN. The patients also received a once-daily dose of 12mcg/kg Elzonris in the first five days of a 21-day cycle. One of the patients achieved a complete response and one clinical complete response in the study.
Some common adverse events noticed in patients during the clinical trials were capillary leak syndrome, nausea, weight gain, fatigue, peripheral oedema and an increase in body temperature.