FETROJA® (cefiderocol) is the first approved siderophore cephalosporin antibacterial drug.
It is indicated for the treatment of complicated urinary tract infections (cUTI), hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) caused by susceptible gram-negative microorganisms such as Escherichia coli (E.coli), Klebsiella pneumoniae, Pseudomonas aeruginosa or Serratia marcescens in the patients aged 18 years and older.
FETROJA is available as white to off-white, sterile, one gram of cefiderocol lyophilised powder for reconstitution in a clear single-dose glass vial for intravenous (IV) infusion.
FETROJA approvals
Developed by Shionogi, the initial new drug application (NDA) for cefiderocol was submitted to the US Food and Drug Administration (FDA) for the treatment of cUTI, including pyelonephritis in December 2018.
The European Medicines Agency (EMA) accepted Shionogi’s marketing authorisation application (MAA) for the drug for review in March 2019.
The FDA approved FETROJA (cefiderocol) for the treatment of cUTI in November 2019. It was designated as an FDA’s Qualified Infectious Disease Product (QIDP), receiving fast track and priority review status.
In Europe, the drug received marketing authorisation under the brand name FETCROJA for the treatment of infections due to aerobic gram-negative bacteria in adults with limited treatment options in April 2020.
The FDA accepted a supplemental NDA (sNDA) for the drug to treat HABP / VABP under priority review status in June 2020, while the drug was approved for the indication in September 2020.
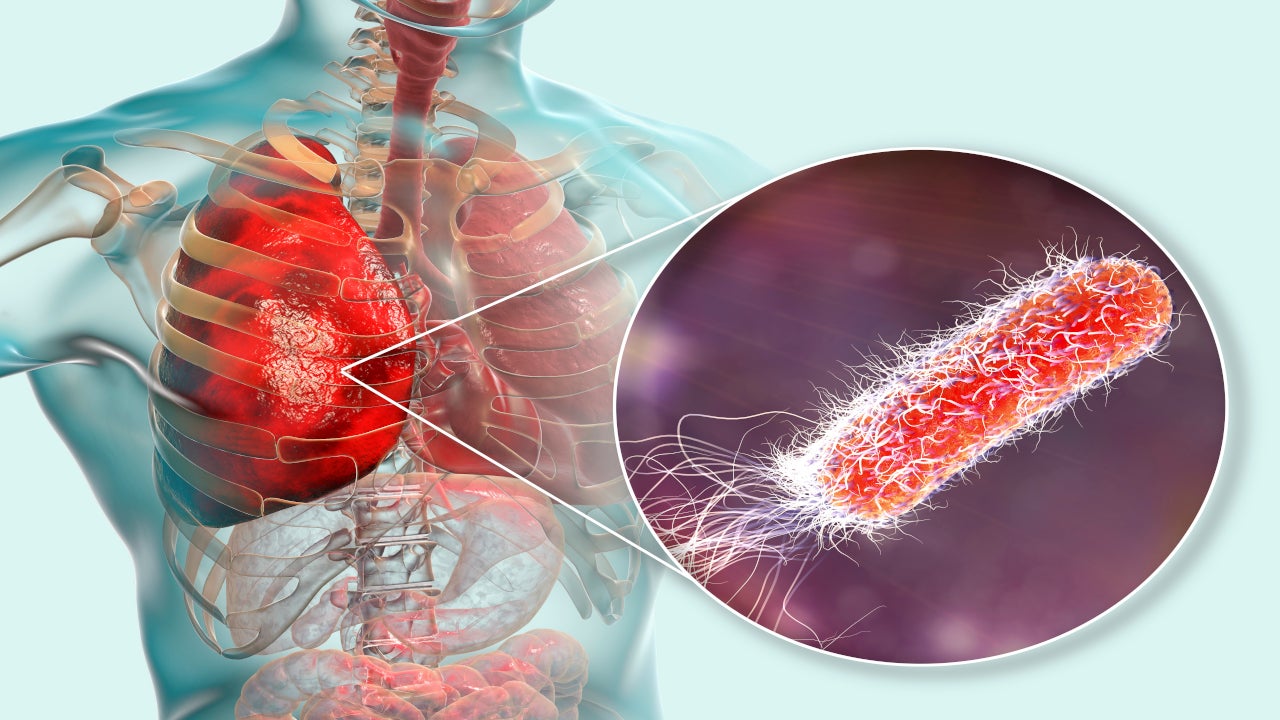
HABP (Nosocomial pneumonia) and VABP causes and symptoms
Nosocomial pneumonia is one of the most common hospital-acquired infections caused by difficult-to-treat, multidrug-resistant pathogens, which can be fatal to patients.
Hospital-acquired (HAP) pneumonia progresses at least 48 hours after admission to the hospital while Ventilator-associated pneumonia (VAP) occurs after at least 48 hours of endotracheal intubation.
The most common cause of both HAP and VAP is micro-aspiration of bacteria colonising in the oropharynx and upper respiratory tract of severely diseased patients.
The most common pathogens causing the diseases are gram-negative bacilli and Staphylococcus aureus as well as other antibiotic-resistant microorganisms. Antibiotic-resistant infections affect more than 2.8 million people a year in the US, leading to more than 35,000 deaths.
Signs and symptoms of HAP include fever, cough, chest pain, malaise, chills and rigour. Fever and elevated respiratory or heart rate, or changes in respiratory parameters, such as a rise in purulent secretions or a worsening of hypoxemia are the symptoms of VAP.
Cefiderocol mechanism of action
Cefiderocol is the cephalosporin antibiotic, which functions as siderophore penetrating the outer cell membrane of gram-negative pathogens, including carbapenem-resistant strains. It enters the cells through porin channels by a passive diffusion mechanism.
Additionally, the drug binds to extracellular free (ferric) iron and is effectively transported into bacterial cells via the outer membrane by bacterial iron transporters, which transport the iron nutrient for bacteria. This results in a high concentration of cefiderocol in the periplasmic space of the bacteria where it attaches to penicillin-binding proteins (PBPs) and blocks the cell wall synthesis activity in bacterial cells (bactericidal).
Cefiderocol also exhibited in vitro activity against specific bacteria with troublesome resistant enzymes such as ESBLs, AmpCs, serine-and Metallo-carbapenemases.
No clinically significant in vitro activity has been established for the drug against most gram-positive bacteria and anaerobic bacteria.
Clinical trials on FETROJA
FDA approval of FETROJA is based on the results of the multinational, multi-centre, double-blind, randomised phase three clinical trial, APEKS-NP.
The trial was intended to determine the safety and efficacy of FETROJA in the treatment of nosocomial pneumonia, including HABP, VABP, and healthcare-associated bacterial pneumonia (HCABP).
In the study, 298 hospitalised patients with HABP / VABP were randomised to receive two grams of FETROJA in every eight hours as a three-hour infusion to meropenem.
Patients in both the treatment groups were administered linezolid 600mg every 12 hours for at least five days to provide coverage for Staphylococcus aureus (MRSA) resistant to methicillin and gram-positive bacteria.
The primary goal of the study was all-cause mortality (ACM) rate in patients on day 14. The ACM in the patients receiving FETROJA was 12.4%, while the rate was 12.2% for high-dose meropenem-receiving patients on day 14.
At day 28, the ACM was 22.1% in FETROJA-receiving patients and 21.1% in patients receiving meropenem.
The most common adverse reactions reported in patients receiving FETROJA were diarrhoea, atrial fibrillation, hypomagnesaemia, elevations in liver tests and hypokalaemia.