Leqvio (inclisiran) is a first-in-class small interfering ribonucleic acid (siRNA) treatment indicated as an adjunct to diet for the treatment of hypercholesterolaemia or mixed dyslipidaemia in adult patients.
The drug can also be used for the reduction of low-density lipoprotein cholesterol (LDL-C) in patients with primary hyperlipidemia (high LDL-C) including heterozygous familial hypercholesterolemia (HeFH).
The drug is designed to reduce elevated LDL-C levels in patients with atherosclerotic cardiovascular disease (ASCVD) or who are at risk of ASCVD, or who had previously experienced a cardiovascular event such as a heart attack or stroke. It is the first and only US Food and Drug Administration (FDA) approved siRNA treatment to lower LDL-C.
Inclisiran was originally developed by US-based RNAi therapeutics company Alnylam Pharmaceuticals, which collaborated with The Medicines Company (TMC) in 2013 to advance clinical trials for the drug and support its potential commercialisation.
In January 2020, Swiss pharmaceutical company Novartis acquired TMC, along with the global rights to develop, manufacture and market Leqvio, under a licence and partnership agreement with Alnylam.
Leqvio is available as a 284mg clear, colourless to pale yellow injectable solution in a prefilled syringe for subcutaneous administration.
Patients need to be administered two maintenance doses a year, following an initial dose and another at three months.
Regulatory approvals for Leqvio
In October 2020, Leqvio received a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use to treat adults with hypercholesterolaemia or mixed dyslipidaemia. The European Commission granted marketing authorisation for the drug in December 2020.
Around this time, Novartis received a complete response letter (CRL) regarding a new drug application (NDA) submitted for inclisiran to the FDA due to unresolved facility inspection-related conditions at a third-party manufacturing facility.
Novartis resubmitted the NDA to the FDA in July 2021, addressing the CRL. The company’s resubmission included details of its facility at Schaftenau, Austria, where it planned to manufacture the drug.
In December 2021, Leqvio received approval from the FDA review for treating adults with elevated LDL-C who are on a maximally tolerated statin regimen.
In August 2021, Novartis signed a commercial agreement with the UK’s National Health Service to make Leqvio accessible to eligible patients across England through a population health management approach.
The FDA expanded the label for Leqvio to include treatment of adults with high LDL-C and who have an increased risk of heart disease, as an adjunct to diet and statin therapy, in July 2023.
The patient population eligible for the treatment encompasses those with comorbidities such as hypertension and diabetes and who have not yet had a first cardiovascular event.
Furthermore, the Limitation of Use statement and four adverse events from the safety section have been removed from the label, based on the extensive VictORION clinical trial programme reaffirming the strong safety and effectiveness data for Leqvio.
VictORION is one of the largest cardiovascular clinical trial programmes designed to generate data consistently and comprehensively. It comprises more than 20 trials, recruiting 47,000 patients in over 50 countries worldwide.
ASCVD causes and symptoms
Atherosclerosis is characterised by the accumulation of lipids in the inner lining of the arteries over time, primarily LDL-C. An atherosclerotic cardiovascular event such as a heart attack or stroke can be caused by an unexpected rupture of the atherosclerotic plaque.
Long-term elevated LDL-C is a recognised cause of ASCVD and a significant risk factor for cardiovascular disease.
More than 85% of all cardiovascular disease fatalities are caused by ASCVD, which is the leading cause of mortality in the EU.
Conditions with a comparable risk of ASCVD occurrences, such as diabetes and heterozygous familial hypercholesterolaemia, are referred to as ASCVD risk equivalents.
Leqvio’s mechanism of action
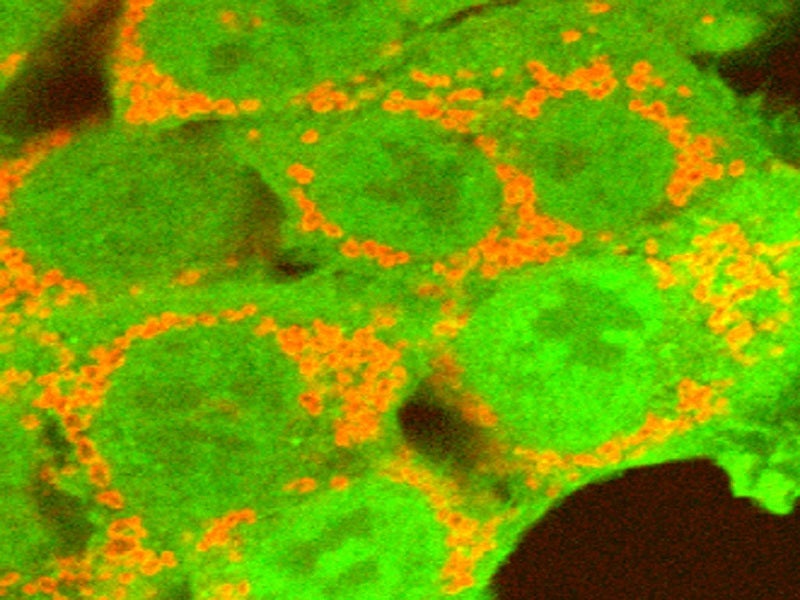
Leqvio is a cholesterol-reducing, double-stranded siRNA coupled with triantennary N-acetylgalactosamine on the sense strand to aid hepatocytes uptake.
The drug’s active ingredient, inclisiran, interferes with RNA (genetic material) to inhibit the development of proprotein convertase subtilisin Kexin type 9 (PCSK9), a protein that can raise LDL cholesterol levels. Leqvio reduces LDL cholesterol levels by inhibiting PCSK9 synthesis.
In hepatocytes, inclisiran uses the RNA interference mechanism to guide catalytic mRNA breakdown for PCSK9. The process enhances LDL-C receptor recycling and expression on the hepatocyte cell surface, increasing LDL-C uptake and decreasing LDL-C levels in blood circulation.
Clinical trials on Leqvio
The FDA’s approval of Leqvio was based on results from a placebo-controlled, double-blind, randomised Phase III clinical trial development programme, which included the ORION-9, ORION-10 and ORION-11 trials.
The global ORION-9 trial was conducted at 46 sites across eight countries. The ORION-10 trial was held at 145 sites in the US, while ORION-11 was carried out at 70 sites across seven countries.
The trials evaluated the efficacy, safety and tolerability of Leqvio sodium salt 300mg, which is equivalent to 284mg of Leqvio when administered subcutaneously by a healthcare professional.
Leqvio showed an effective and sustained decrease in LDL-C level of up to 52% in patients with elevated LDL-C, despite maximally tolerated statin therapy. The drug is expected to support long-term adherence with two doses a year.
In ORION-9, 482 patients with clinical or genetic evidence of HeFH were recruited. Inclisiran was administered three months after the initial dose, followed by one every six months. This reduced the mean percentage change in LDL-C by 48% compared to placebo at 17 months.
The ORION-10 and ORION-11 trials were conducted in patients with ASCVD and ASCVD risk equivalents.
A total of 1,561 participants with ASCVD were enrolled in ORION-10. In the study, Leqvio demonstrated a mean percentage change in LDL-C reductions of 52% compared to placebo at 17 months, and a time-adjusted percentage change in LDL-C reductions of 54% from three to 18 months.
The ORION-11 study evaluated 1,617 patients with ASCVD or ASCVD risk equivalents, in which Leqvio significantly lowered the mean percentage change in LDL-C by 50% compared to placebo.
Common adverse events reported among the patients treated with Leqvio during the trials were injection site reaction, arthralgia, urinary tract infection, diarrhoea, bronchitis, pain in extremities, and dyspnoea.
ORION-3 clinical trial details
ORION-3, a part of the VictORION study, was a four-year open-label extension study of the Phase II ORION-1 trial, which evaluated the safety and efficacy of Leqvio in 233 patients with ASCVD.
The primary endpoint of the study was the percentage LDL-C change from baseline (Day 1 of ORION-1) to day 210 of ORION-3.
In the study, the patients treated with Leqvio maintained a significant reduction in LDL-C levels over a four-year period. The average reduction in LDL-C from baseline to Day 210 was 47.5%. Additionally, the time-averaged reduction in LDL-C over the four years, achieved through twice-yearly dosing, was 44.2%.
The results indicate the sustained effectiveness of Leqvio in lowering LDL-C levels over an extended treatment period.
After a four-year therapy period, Leqvio exhibited good tolerability and maintained a safety profile similar to the findings from previous 18-month Phase III studies focused on lowering LDL-C levels.
General disorders and injection site reactions were the most common adverse effects reported in the patients during the clinical trial.