Omvoh™ is the first and the only treatment for moderate to severe active ulcerative colitis (UC) in adults that specifically targets interleukin-23p19 (IL-23p19), a key player in inflammation associated with UC.
Developed by Eli Lilly, a US-based pharmaceutical company, Omvoh provides relief from three key symptoms, stool frequency, rectal bleeding, and bowel urgency, irrespective of the previous biologic use.
Omvoh is clear to opalescent, colourless to a slightly yellow to slightly brown solution available in 300mg/15ml (20mg/ml) strength in a single-dose vial for intravenous infusion, as well as 100mg/ml solution in a single-dose prefilled pen for subcutaneous use.
Regulatory approvals for Omvoh
Omvoh was first approved in Japan in March 2023 for use as induction and maintenance therapy in patients with moderate to severe UC who have an inadequate response to conventional treatments.
The drug received a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) in the same month and was granted marketing authorisation in the European Union (EU) for the indication in May 2023.
In October 2023, the US Food and Drug Administration (FDA) approved Omvoh for treating adults with moderate to severe active UC.
The drug is also indicated for the treatment of the same condition in Germany, the UK and Canada.
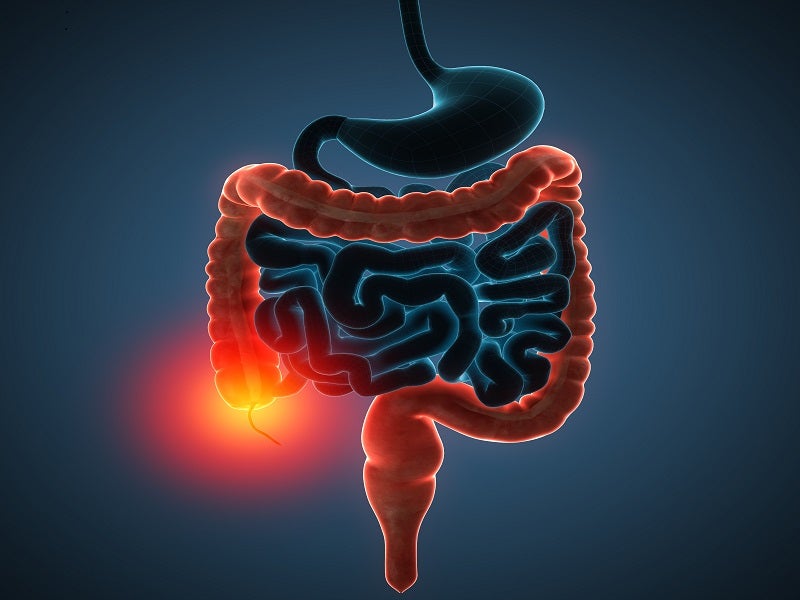
Ulcerative colitis causes and symptoms
UC is a chronic inflammatory bowel condition characterised by large intestine and rectum inflammation.
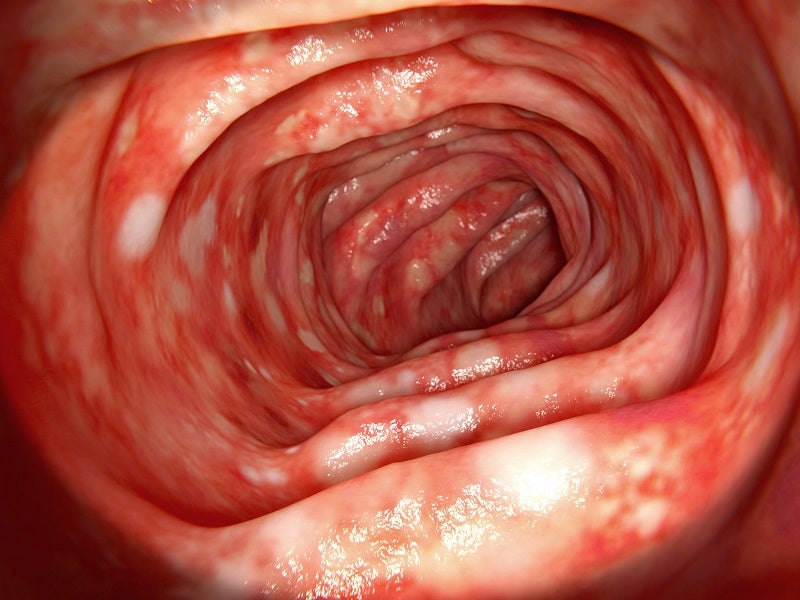
Its cause is unknown, but research indicates that immune system malfunction causes inflammation and ulcers on the inner lining of the large intestine. Heredity is another factor that causes UC in certain cases with family history.
UC is categorised into four types, namely ulcerative proctitis, proctosigmoiditis, left-sided colitis and pancolitis.
Its symptoms can vary depending on the severity of inflammation and the area of occurrence. Typical symptoms of the disease include abdominal pain, bloody diarrhoea, mild to severe bowel urgency, incontinence, rectal pain, fever, weight loss and fatigue.
Omvoh’s mechanism of action
Mirikizumab-mrkz is a humanised IgG4 monoclonal antibody that selectively binds to the specific protein p19 subunit of human IL-23 cytokine and inhibits the IL-23 pathway. Inflammation due to over-activation of the IL-23 pathway plays a critical role in the pathogenesis of UC.
IL-23 plays a role in mucosal inflammation, influencing the differentiation, expansion, and survival of T cell subsets and innate immune cell subsets, representing sources of pro-inflammatory cytokines.
Mirikizumab-mrkz blocks the release of pro-inflammatory cytokines and chemokines.
Clinical trials on Omvoh
The FDA approval of Omvoh was based on the positive outcomes from the LUCENT programme, which includes two randomised, double-blinded, placebo-controlled phase III clinical trials with a 12-week induction study (UC-1) and a 40-week maintenance study (UC-2) totalling to 52 weeks of continuous treatment.
The study evaluated the safety and efficacy of Omvoh in adults with moderately to severely active UC, who are biologic-naive, and harder-to-treat patients and had previously taken a biologic that failed.
In the UC-1 study, enrolled patients were randomised to a 3:1 ratio to receive either 300mg intravenous (IV) Omvoh or a placebo IV every four weeks, for 12 weeks. Participants who demonstrated a clinical response at week 12 with Omvoh in UC-1 were randomly assigned in a 2:1 ratio to receive either a 200mg subcutaneous injection of Omvoh or a placebo subcutaneous injection every four weeks for an additional 40 weeks in UC-2.
The primary endpoint of UC-1 and UC-2 was clinical remission at weeks 12 and 52, respectively.
In the UC-1, out of all the patients treated with Omvoh, 65% achieved clinical response compared to 43% of placebo while approximately 24% achieved clinical remission compared to 15% of placebo.
In UC-2, 51% of the patients treated with Omvoh achieved clinical remission compared to 27% of placebo at 40 weeks.
The studies showed significant improvements in rectal bleeding and stool frequency as early as three weeks in patients receiving Omvoh compared to placebo.
The most common adverse reactions reported in the patients during the clinical trials were upper respiratory tract infections, injection site reactions, arthralgia, rash, headache, and herpes viral infection.
The drug is also being evaluated in a Phase III clinical study named VIVID-1 for Crohn’s disease.