Oritavancin is an investigational glycopeptide antibiotic being developed by Targanta Therapeutics for the treatment of serious gram-positive bacterial infections. It was originally discovered and developed by scientists at Eli Lilly as a potential replacement for vancomycin. Targanta Therapeutics acquired worldwide rights to oritavancin from Intermune Inc in 2005, to which the drug had previously been licensed in 2001.
Targanta submitted a marketing authorization application (MAA) for oritavancin to the European Medicines Agency (EMEA). In June 2008, EMEA accepted the MAA for review.
In February 2008, Targanta filed a new drug application (NDA) with the US Food and Drug Administration (FDA) for the use of oritavancin in the treatment of complicated skin and soft tissue infections (cSSIs). Other potential indications for this new antibiotic include bacteraemia and osteomyelitis.
In December 2008, the FDA rejected Targanta’s NDA for oritavancin. In its reply to Targanta’s application, the FDA stated that oritavancin did not exhibit safety and effectiveness for the treatment of cSSIs.
The FDA found that the two clinical trials submitted by Targanta were not sufficient for approval. It stated that Targanta should conduct additional studies to prove the drug’s efficacy in treating MRSA. The FDA also suggested that Targanta should track macrophage function and phlebitis rates.
Following the FDA’s rejection, Targanta planned to conduct another study by enrolling patients with MRSA. The new trials are expected to take at least two years to complete and cost the company $20m. As a result, Targanta is looking for funding opportunities, including partnership with a biotech or pharmaceutical company. Targanta also underwent restructuring of its operations by cutting down 75% of its workforce.
Meeting the challenge of gram-positive resistance
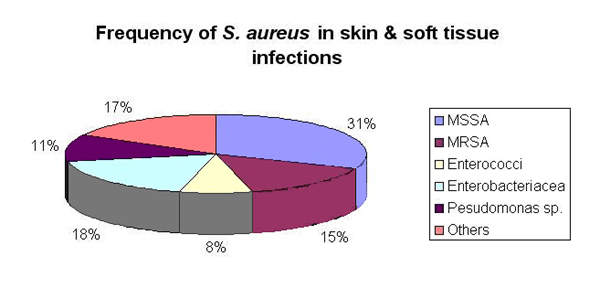
The emergence of strains of gram-positive bacteria such as Streptococcus pneumoniae, Staphylococcus aureus, Staphylococcus epidermidis and enterococci resistant to common antibiotics poses a major therapeutic challenge.
For many years the glycopeptide vancomycin was the mainstay of treatment of infections such as methicillin-resistant S aureus (MRSA) and difficult-to-treat enterococcal infections.
However, reduced susceptibility of S aureus to vancomycin and resistance to vancomycin among strains of enterococci now limit its clinical usefulness.
The advent of the oxazolidinone, linezolid, and the streptogramin combination, quinupristin-dalfopristin, as well as more recent additions such as the glycylcycline tigecycline and glycopeptide, dalbavancin have expanded treatment options for serious resistant gram-positive infections.
However, evidence has emerged of resistance to linezolid and quinupristin-dalfopristin; additionally, quinupristin-dalfopristin lacks intrinsic activity against Enterococcus faecalis. Consequently there remains a need for more agents to combat multidrug-resistant gram-positive infections.
Glycopeptides a growing class of antibiotics
The glycopeptides are an important class of antibiotics for the treatment of serious gram-positive infections, including those due to staphylococci and enterococci. Today this class contains not only vancomycin, approved by the FDA in 1964, but also teicoplanin and dalbavancin.
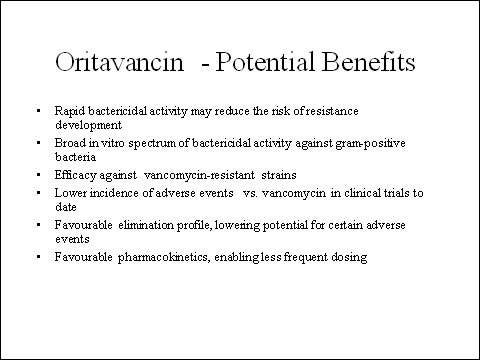
Oritavancin is semi-synthetic derivative of a precursor drug closely related to vancomycin. Although it has a similar mode of action to vancomycin, important differences exist such as that oritavancin has activity against vancomycin-resistant pathogens. For example, oritavancin inhibits the transglycosylation step of bacterial cell-wall biosynthesis.
In contrast to vancomycin, oritavancin possesses concentration-dependent bactericidal activity against enterococci, S pneumoniae, and staphylococci, including MRSA. Importantly, it is not affected by the vanA, vanB, and vanC-encoded alterations in the bacterial cell wall that confer vancomycin resistance.
Efficacy in cSSIs
Oritavancin has demonstrated clinical effectiveness in two pivotal Phase III trials in patients with cSSIs due to gram-positive pathogens. The first was a 517-patient randomised, double-blind, parallel-group trial, in which three-days i.v. oritavancin (1.5 and 3.0mg/kg/day) was compared with i.v. vancomycin 10–15mg/kg twice daily for three to seven days followed by oral cephalexin 500–1,000mg twice daily to complete up to 14 days therapy.
The second trial, of similar design, enrolled 1,267 patients with cSSIs who were randomised to either i.v. oritavancin 200mg/day for three to seven days followed by oral placebo, or i.v. vancomycin 15mg/kg twice/day for three to seven days followed by oral cephalexin 1,000mg twice daily.
In both trials the primary endpoint (clinical cure in clinically evaluable patients at first follow-up with 10% non-inferiority margin) was met with the advantage of a shorter duration of therapy for patients in the oritavancin treatment arm. In the larger of the two trials, treatment with oritavancin was associated with a 19.2% relative reduction in the overall incidence of adverse events compared with vancomycin/cephalexin (p<0.001).
Marketing commentary
In an era of rising rates of bacterial resistance to commonly used antibiotics, new agents are urgently needed to treat bacterial infections effectively and halt the spread of resistant strains.
This need is arguably greatest in the hospital environment where rates of bacterial resistance are highest. MRSA is a particular problem because it displays resistance to most classes of antibiotics.
Although the hospital antibacterial market represents only a third of all antibacterial sales, increasing antibiotic resistance in the hospital environment has increased the demand for more effective antibiotics making it an attractive sector for new antibacterial agents.