Rituxan (rituximab) is a prescription medicine indicated to treat blood cancers, autoimmune diseases and inflammatory conditions, including follicular lymphoma (FL), non-Hodgkin’s lymphoma (NHL), diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL), Burkitt-like lymphoma (BLL), or mature B-cell acute leukaemia (B-AL), chronic lymphocytic leukaemia (CLL), rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA), and pemphigus vulgaris (PV).
RITUXAN HYCELA (rituximab and hyaluronidase human) injection is a combination of rituximab and Halozyme’s hyaluronidase human ENHANZE technology indicated for the treatment of adults with previously untreated and relapsed or refractory FL, previously untreated DLBCL, and previously untreated and previously treated CLL.
The technology helps to deliver the drug under the skin.
Rituxan was developed by Biogen Idec, a biotechnology company based in the US, together with the copromotion partner Genentech, a subsidiary of Roche Group. The companies market the drug in the US.
Roche markets the drug under the brand name MabThera in the rest of the world, except Japan, where Rituxan is marketed by Japanese pharmaceutical companies Zenyaku Kogyo and Chugai Pharmaceutical. In Roche’s pipeline, Rituxan is the second largest-selling drug after the anti-cancer drug Avastin.
Rituxan is a clear, colourless solution for intravenous infusion, available in single-dose vials of 100mg/10ml and 500mg/50ml.
On the other hand, RITUXAN HYCELA is a colourless to yellowish, clear to opalescent solution for subcutaneous injection.
It is available in single-dose vials containing 1,400mg rituximab and 23,400 units of hyaluronidase human per 11.7ml and 1,600mg rituximab and 26,800 units of hyaluronidase human per 13.4ml.
Regulatory approvals for Rituxan
In December 2021, the US Food and Drug Administration (FDA) approved Rituxan with chemotherapy for paediatric patients aged six months to 18 years with certain advanced-stage lymphomas, DLBCL, BL, BLL, or mature B-AL, based on the Inter-B-NHL Ritux 2010 trial.
In September 2019, the FDA authorised Rituxan with glucocorticoids for the first paediatric indication to treat autoimmune diseases PA and MPA in children aged two and older, based on the PePRS study.
In June 2018, the FDA approved Rituxan for adults with moderate to severe PV, based on the Ritux 3 trial.
In April 2011, the FDA authorised Rituxan with corticosteroids for Wegener’s granulomatosis and MPA, two severe types of vasculitis known as ANCA-Associated Vasculitis (AAV), based on the RAVE trial.
The FDA approved Rituxan as a maintenance treatment for advanced FL patients who responded to initial treatment, based on the PRIMA study, In January 2011. The European Commission approved it for a similar indication in October 2010.
In February 2010, the FDA approved Rituxan with fludarabine and cyclophosphamide for CLL patients, based on data from two Phase III studies, CLL8 and REACH studies.
The FDA approved Rituxan with methotrexate (MTX) for RA patients who had inadequate response to TNF antagonist therapies, in February 2006.
Rituxan was FDA-approved in 1997 for NHL and received the European Union approval in June 1998, marketed as MabThera.
Regulatory approvals for RITUXAN HYCELA
The FDA approved RITUXAN HYCELA SC injection in June 2017 for the treatment of adults with relapsed or refractory FL, previously untreated DLBCL, and previously untreated and previously treated CLL.
Lymphoma causes and symptoms
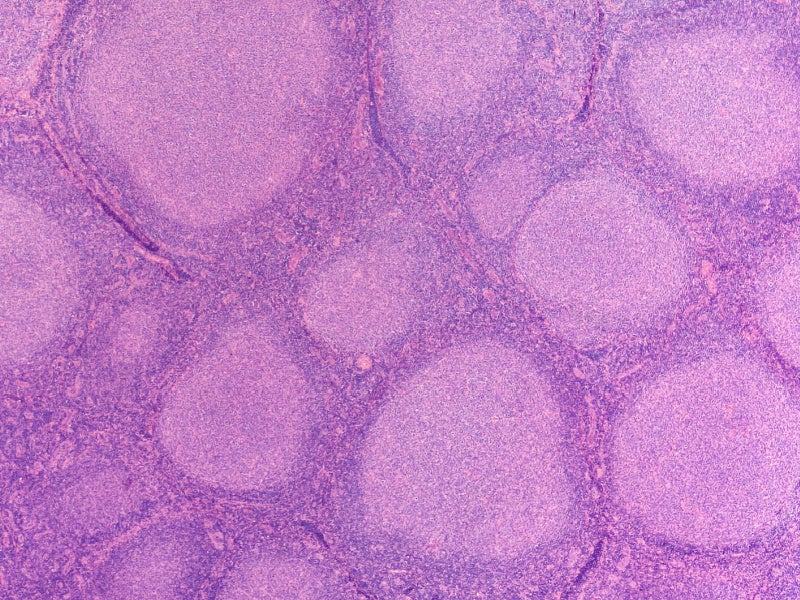
NHL is a cancer affecting lymphocytes, a type of white blood cells, mainly found in lymph nodes but can also involve other areas such as bone marrow, spleen, waldeyer’s ring, and peripheral blood. The median survival is between eight and ten years.
NHLs are categorised as slow-growing (indolent NHL) and fast-growing (aggressive NHL), with the most common types being FL (indolent) and DLBCL (aggressive), which can occur in various parts of the body beyond the lymphatic system.
Symptoms of NHL include swollen lymph nodes, discomfort, abdominal fullness, fatigue, shortness of breath, fever, night sweats, weight loss, and weakness.
CLL is a blood cancer characterised by abnormal lymphocytes in the blood and bone marrow, leading to reduced healthy blood cells and resulting in infections, anaemia, and excess bruising and bleeding. Symptoms include weakness, fatigue, shortness of breath, weight loss, fever, night sweats, enlarged lymph nodes, abdominal pain, infections, and bleeding.
RA is a chronic disease where the immune system attacks the body’s joints and tissues, causing symptoms such as swollen joints, joint tenderness, stiffness, pain, low fever, and symmetrical RA.
AAV is a condition where inflammation in small blood vessels thickens blood vessel walls, reducing blood flow and potentially damaging organs.
The inflammation is often caused by harmful autoantibodies such as ANCAs, targeting neutrophils and causing inflammation and swelling in various organs.
GPA and MPA can have flares and periods of remission, with flares worsening or new symptoms appearing, and remission being a period of controlled or absent symptoms.
Rituxan’s mechanism of action
Rituximab is a monoclonal antibody that specifically targets the CD20 antigen found on the surfaces of pre-B and mature B cells.
When rituximab binds to the receptor, it triggers cell lysis via complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity.
RITUXAN HYCELA contains a combination of human hyaluronidase and rituximab. Hyaluronidase is added to enhance the permeability of subcutaneous tissue by breaking down hyaluronan at the injection site.
Hyaluronan, a polysaccharide in subcutaneous tissue, is depolymerised by hyaluronidase, a naturally occurring enzyme that enhances subcutaneous tissue permeability by briefly depolymerising hyaluronan.
The effects are reversible, and permeability is restored within 24 to 48 hours. Hyaluronidase human has been shown to increase the absorption rate of a rituximab product into the systemic circulation in Göttingen minipigs.
Clinical trials on Rituxan
The FDA approved Rituxan based on the PRIMA (primary Rituxan and maintenance) Phase III clinical trials conducted from December 2004 to May 2007, involving 1,217 FL patients. The open-label, multicentre, randomised study had two treatment phases.
The study assessed the safety and efficacy of Rituxan with chemotherapy in FL patients, focusing on progression-free survival (PFS) time from randomisation to progression, relapse, or death.
Initial treatment comprised eight cycles of Rituxan with various chemotherapies. Responding patients were then randomised to receive Rituxan every two months for two years as a single agent.
Results showed that Rituxan combined with chemotherapy doubled PFS in FL patients. The study confirmed the safety and efficacy of 375mg/m² Rituxan, consistent with previous pivotal studies, whether used alone or with chemotherapy, compared to those not continuing Rituxan.
Common adverse reactions included infections, neutropenia, nausea, constipation, cough, and fatigue.
Additional clinical trials on Rituxan
In December 2010, Roche reported positive results from multicentre, randomised Phase III clinical trials on Rituxan conducted on 462 patients without symptoms of FL.
The study was designed to find the safety and efficacy of Rituxan in three phases. In phase A, the patients were not administered with any therapy but were just observed. In phase B, the patients were administered 375mg/m² of Rituxan weekly for four cycles.
In phase C for four cycles 375mg/m² of Rituxan was administered to the patients followed by Rituxan maintenance, which was given once every two months.
The results of the study demonstrated that immediate use of Rituxan decreased the risk of necessity for additional therapy by 80% and the risk of disease worsening by 79% compared with watchful waiting.
Clinical trials on RITUXAN HYCELA
The FDA approval of RITUXAN HYCELA was based on the results from multiple clinical studies including SABRINA, a Phase III combined chemotherapy and maintenance trial in previously untreated FL patients, SAWYER, a Phase Ib trial in previously untreated CLL, MabEase, a Phase III trial of previously untreated DBCL, and PrefMab, a Phase III patient preference trial for previously untreated FL and DLBCL.
The trials showed comparable clinical efficacy results and non-inferior rituximab levels in the blood.
One study found that the majority (77%) of patients chose RITUXAN HYCELA versus intravenous Rituxan, with the most common reason being that administration took less time in the clinic. RITUXAN HYCELA can only be administered after at least one complete dose of intravenous Rituxan.
The most common adverse reactions for FL, DLBCL, and CLL were infections, neutropenia, nausea, constipation, cough, fatigue, alopecia, anaemia, and injection site erythema, among others.