SPEVIGO® (spesolimab-sbzo) is a first-in-class monoclonal antibody indicated for the treatment of adults with generalised pustular psoriasis (GPP) flares, a rare autoinflammatory skin disease.
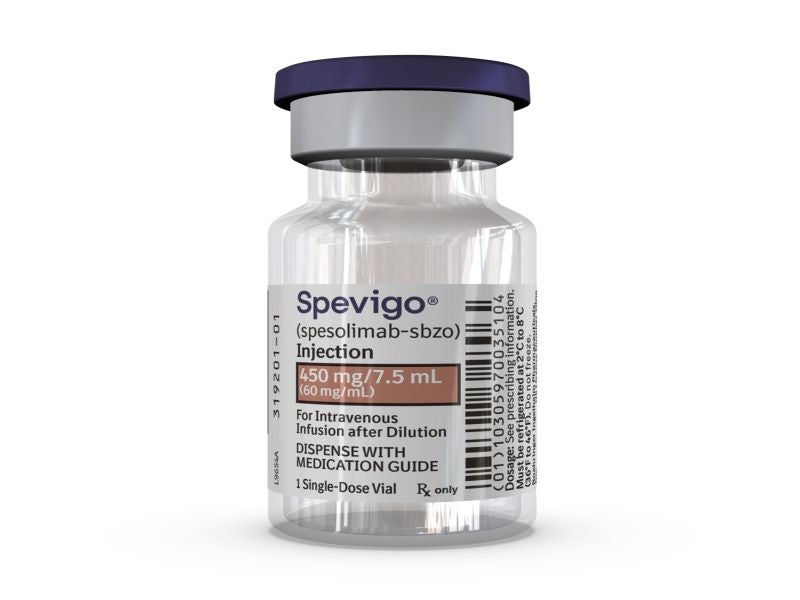
Developed by German pharmaceutical company Boehringer Ingelheim, Spevigo is available as colourless to slightly brownish-yellow, clear to slightly opalescent 450mg/7.5mL (60mg/mL) solution in a single-dose vial for intravenous administration.
Spesolimab is being continuously investigated for the treatment of neutrophilic skin diseases.
Regulatory approvals for Spevigo
In September 2022, the US Food and Drug Administration (FDA) approved Spevigo for the treatment of GPP flares. The drug received conditional marketing authorisation for the condition in Europe in December 2022 and has also been approved in Japan.
The drug has received breakthrough therapy designation in the US, Mainland China and Taiwan, priority review in the US and Mainland China, orphan drug designation in the US, Korea, Switzerland and Australia, and rare disease and fast track designations in Taiwan. Each of these designations is for GPP flare treatment.
Pustular psoriasis flare causes and symptoms
GPP is a rare and potentially life-threatening neutrophilic skin disease characterised by recurrent flares. Also known as von Zumbusch psoriasis, the condition is associated with episodes of widespread eruptions of painful and sterile pustules.
GPP is caused by the accumulation of neutrophils, a type of white blood cell in the skin, which results in pustules developing all over the body. The condition’s exact cause is unknown, but GPP flares can be triggered by overexposure to sunlight, genetic mutations, infections, stress, corticosteroid treatment withdrawal, hormonal changes, and pregnancy.
GPP flares are generally associated with symptoms such as fever, fatigue, muscle weakness, anorexia, nausea, severe pain, increased white blood cells, and other signs of inflammation all over the body.
The condition often appears between 40 and 50 years of age, depending on the individual’s genetic makeup. Its estimated prevalence ranges from 0.27 to 4.6 for every 10,000 people worldwide.
Spevigo’s mechanism of action
Spevigo is a novel, humanised, selective antibody that blocks the activation of the interleukin-36 receptor (IL-36R), a signalling pathway in the immune system that is involved in the pathogenesis of several autoinflammatory diseases, including GPP.
Spesolimab-sbzo inhibits IL-36 signalling by specifically binding to the IL36R, which prevents the subsequent activation of IL36R by cognate ligands (IL-36 α, β and γ) and downstream activation of pro-inflammatory and pro-fibrotic pathways. The exact mechanism that links reduced IL36R activity with the treatment of flares of GPP is not fully understood.
Clinical trials on Spevigo
The FDA’s approval of Spevigo was based on findings from Effisayil 1, a 12-week, randomised, double-blinded Phase II clinical trial that enrolled 53 patients experiencing a GPP flare.
Patients in the Effisayil 1 trial were randomised in a 2:1 ratio to receive either a single intravenous 900mg dose of Spevigo or a placebo. The study’s primary goal was to determine the density of pustules by a GPP Physician Global Assessment (GPPGA) pustulation subscore ranging from zero for no visible pustules to four for severe pustulation at the end of the first week.
After one week, 54% of patients treated with Spevigo showed no visible pustules, compared with 6% of patients who were given placebo.
The most common adverse reactions to Spevigo reported in Effisayil 1 were weakness and fatigue, nausea and vomiting, headache, severe itching leading to prurigo, infusion site haematoma and bruising, and urinary tract infection.