Tivdak™ (tisotumab vedotin-tftv) is a first-in-class antibody-drug conjugate (ADC) indicated for the treatment of recurrent or metastatic cervical cancer in adult patients whose disease has progressed during or after chemotherapy.
The drug is co-developed by Genmab and Seattle Genetics (Seagen) through a commercial license and collaboration agreement signed in October 2011. Seagen exercised its option to co-develop and market the drug in August 2017.
Seagen will commercialise Tivdak in the US, Canada and Mexico, while Genmab will be responsible for commercialising the drug in all other regions.
In February 2021, a biologics license application (BLA) for Tivdak was submitted to the US Food and Drug Administration (FDA) seeking accelerated approval. The BLA was accepted with priority review in April 2021 and approved in September 2021.
The drug is available as a sterile, white to off-white lyophilised cake or powder in a single-dose vial containing 40mg of tisotumab vedotin-tftv for reconstitution. Its recommended dose is 2mg/kg administered intravenously for 30 weeks and every three weeks.
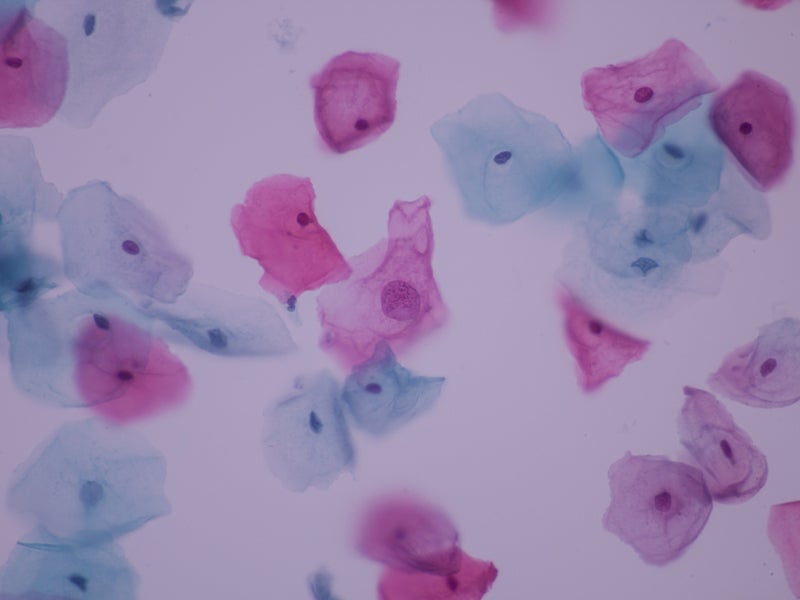
Cervical cancer causes and symptoms
Cervical cancer originates in the cell lining tissues of the cervix, at the lower and narrow end of the uterus, mostly due to human papillomavirus (HPV) infection. The disease usually develops slowly over time.
The signs and symptoms of cervical cancer include vaginal bleeding, unusual vaginal discharge, pelvic pain, and pain during sexual intercourse.
Cervical cancer is the most prominent cause of cancer death in women worldwide, accounting for around 311,000 deaths in 2018.
It is estimated that more than 14,480 new cases of invasive cervical cancer and 4,290 cervical cancer deaths will occur in the US in 2021.
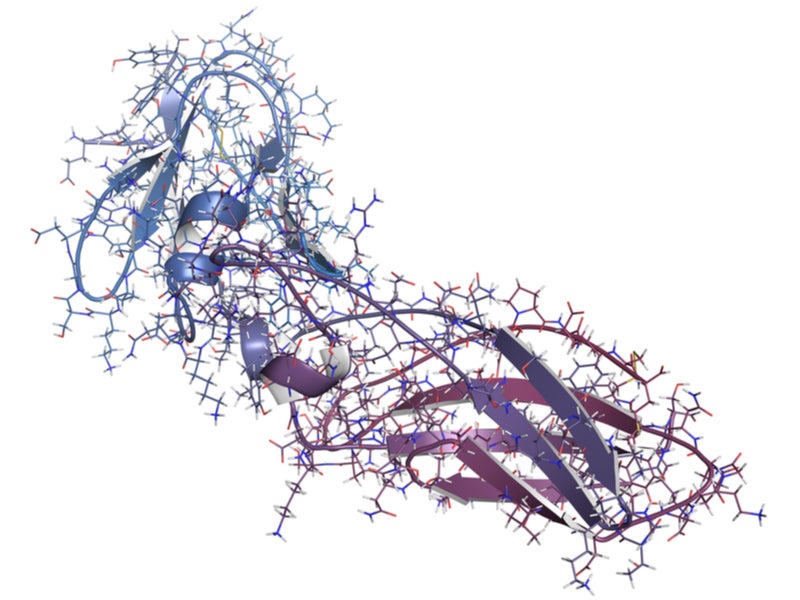
Tivdak’s mechanism of action
Tivdak works as a tissue factor (TF) directed ADC. The human IgG1-kappa antibody targets the cell surface TF protein, the prime initiator of the extrinsic blood coagulation cascade. TF plays a role in tumour signalling and angiogenesis.
The antibody is attached to a small molecule, monomethyl auristatin E (MMAE), which is a microtubule-disrupting agent, through a protease-cleavable vc (valine-citrulline) connector, forming the ADC.
The ADC binds to TF expressing cancer cell surface, followed by the complex internalisation of ADC-TF and release of MMAE through proteolytic cleavage. MMAE breaks the microtubule network of actively dividing cells, resulting in cell cycle arrest and apoptotic cell death.
In addition, Tivdak facilitates antibody-dependent cellular phagocytosis and cytotoxicity in-vitro.
Clinical trials on Tivdak
The FDA’s accelerated approval of Tivdak was based on an open-label, multi-centre, single-arm Phase II clinical trial, innovaTV 204.
The trial evaluated Tivdak’s efficacy in 101 recruited patients with recurrent or metastatic cervical cancer receiving no more than two prior systemic regimens, with at least one previous platinum-based chemotherapy treatment regimen.
Patients were given 2mg/kg of Tivdak every three weeks until disease progression or unacceptable toxicity.
The primary outcome measure of the trial was objective response rate (ORR) evaluated by an independent review committee (IRC) using RECIST v1.1 criteria and duration of response (DOR).
Results demonstrated the confirmed ORR of 24%. Of this, 7% of patients achieved a complete response, while 17% of patients achieved a partial response. The median DOR observed in patients was 8.3 months.
The secondary endpoints were progression-free survival (PFS), overall survival (OS), and safety and tolerability. The median PFS was 4.2 months, while the median OS was 12.1 months. The PFS and OS rates at six months were 30% and 79% respectively.
The most frequent adverse effects reported in patients during the clinical trial were decreased lymphocytes and leukocytes, fatigue, alopecia, haemorrhage, decreased haemoglobin levels, nausea, increased creatinine, epistaxis, diarrhoea, peripheral neuropathy, conjunctival adverse reactions, dry eye, rashes, prolonged activated partial thromboplastin time, and increased prothrombin international normalised ratio.