VOXZOGO™ (vosoritide) is a once-daily therapeutic medicine indicated for the treatment of achondroplasia in children aged five years and older with open growth plates by improving their linear growth.
Developed by BioMarin Pharmaceutical, the drug is available as a white to yellow lyophilised powder in a single-dose vial in 0.4mg, 0.56mg, or 1.2mg dosage strengths. It is administered subcutaneously after reconstitution.
Regulatory approvals for VOXZOGO
In August 2021, Vosoritide was approved in Europe, becoming the first medicine approved in the continent to treat children with achondroplasia.
The US Food and Drug Administration (FDA) granted accelerated approval to VOXZOGO in November 2021.
In June 2022, Japan’s Ministry of Health, Labour and Welfare (MHLW) approved VOXZOGO for achondroplasia without any lower age limit for treatment.
The drug has also received approval in Brazil and is being reviewed for marketing approval in Australia.
Achondroplasia signs and symptoms
Achondroplasia is a lifelong genetic condition that occurs due to a mutation in the fibroblast growth factor receptor 3 (FGFR3) gene, which is a negative bone growth regulator. It is a common form of skeletal dysplasia that leads to disproportionate dwarfism.
The condition is characterised by the slowing of endochondral bone growth and disproportionate development of long bones, spine, face, and skull base.
Achondroplasia causes generalised abnormalities in the cartilage and bone of an individual and affects muscle, tendons and ligaments significantly. People with the condition have short hands, short limbs, hyperlordosis, and macrocephaly with saddle nose, high forehead and normal intellectual ability.
They may also suffer from neurologic problems such as cervicomedullary myelopathy, hydrocephalus, and spinal cord myelopathy.
A full medical history and physical examination can be used to diagnose the condition either before or after birth using foetal ultrasonography. A prenatal DNA test is available for parents who are more likely to have an achondroplasia-affected child.
VOXZOGO’s mechanism of action
The FGFR3 gene, which controls growth, is permanently ‘turned on’ in achondroplasia patients, hindering the normal formation of bones and resulting in shorter-than-normal bones.
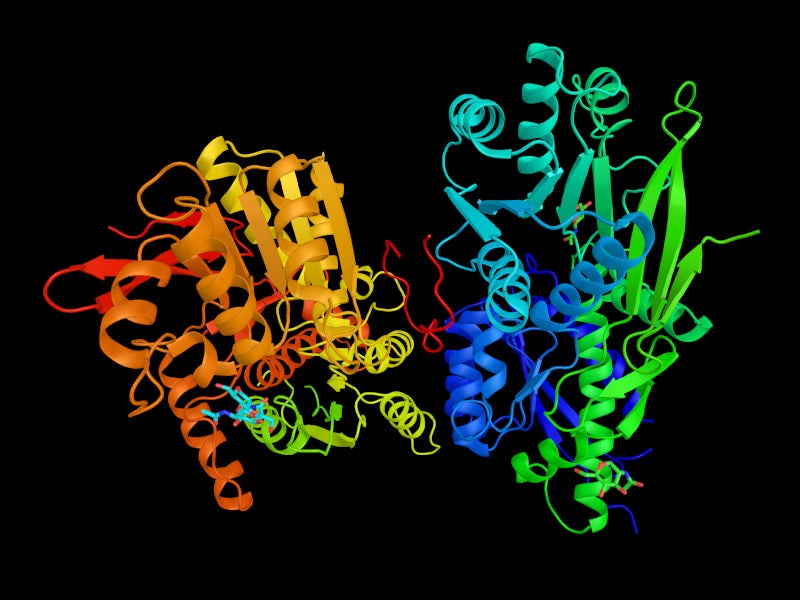
VOXZOGO is a modified C-type natriuretic peptide (CNP), which binds to the receptor called natriuretic peptide receptor-B (NPR-B) and antagonises FGFR3 downstream signalling by inhibiting the extracellular signal-regulated kinases 1 and 2 (ERK1/2) in the mitogen-activated protein kinase (MAPK) pathway and accelerate fibrosarcoma serine/threonine (RAF-1).
As a result, the drug acts as a positive regulator of endochondral bone growth by inhibiting FGFR3 function. It promotes chondrocyte growth and differentiation.
Clinical trials on VOXZOGO
VOXZOGO’s safety and efficacy were evaluated in a 52-week global randomised, double-blind, placebo-controlled, Phase Ⅲ clinical trial, which enrolled 121 genetically confirmed achondroplasia patients aged five to 14.9 years. The study was followed by an open-label extension study.
In the 52-week study, the patients were randomised to receive either a once-daily injection of 15mcg/kg VOXZOGO or a placebo.
The study’s primary efficacy endpoint was the annualised growth velocity (AGV) in patients at 52 weeks compared with placebo. At 52 weeks, patients treated with VOXZOGO showed a statistically significant improvement in AGV of 1.57cm/year compared with those given placebo.
A total of 58 patients initially randomised to receive VOXZOGO were enrolled in an open-label extension study after the 52-week study. The improvements in AGV shown in the 52-week study were maintained in patients who had had two years of follow-up since randomisation.
The most common side effects observed in the patients during the clinical trial were injection site reactions, low blood pressure, arthralgia, vomiting, and gastroenteritis.