Xenpozyme® (olipudase alfa) is an enzyme replacement therapy indicated to treat non-central nervous system (CNS) conditions of acid sphingomyelinase deficiency (ASMD), a rare and progressive genetic condition, in both paediatric and adult patients.
Xenpozyme is developed and marketed by Genzyme, a fully owned subsidiary of Sanofi. The drug is available as a 20mg white to off-white lyophilised powder in vials for concentrate for solution for infusion.
Regulatory approvals for Xenpozyme
In March 2022, Japan’s Ministry of Health, Labour and Welfare (MHLW) approved Olipudase alfa under the SAKIGAKE fast-track designation to treat ASMD.
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) recommended the approval of Xenpozyme for the treatment of non-CNS manifestations of ASMD type A/B or type B in Europe in May 2022, following its receipt of PRIority MEdicines (PRIME) designation by the EMA. Xenpozyme has not yet been studied in patients with ASMD type A.
Xenpozyme received marketing approval in the European Union in June 2022.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to olipudase alfa and has accepted a biologics license application (BLA) for the drug for priority review. A decision is expected in October 2022.
Acid sphingomyelinase deficiency (ASMD) causes and symptoms
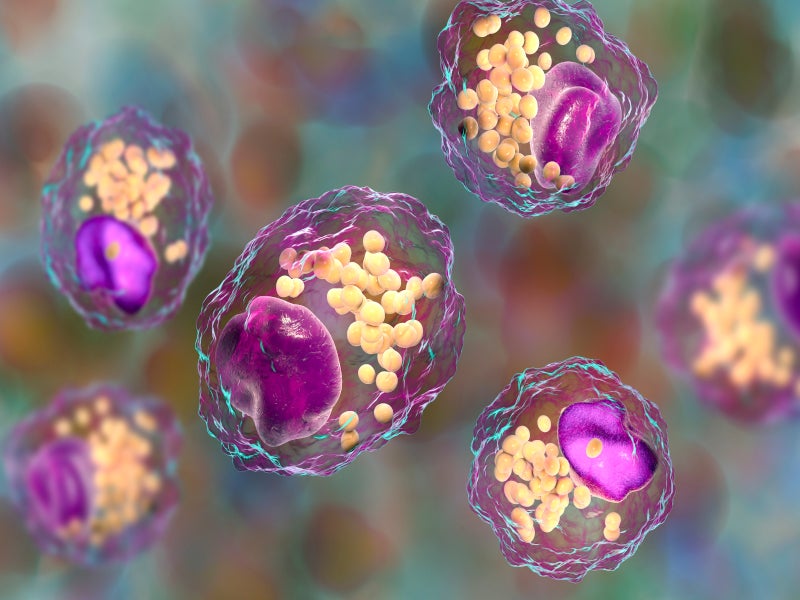
ASMD, also known as Niemann-Pick disease, is a rare lipid storage disorder caused by a deficiency of the enzyme acid sphingomyelinase (ASM). The enzyme is required to break down lipids called sphingomyelin.
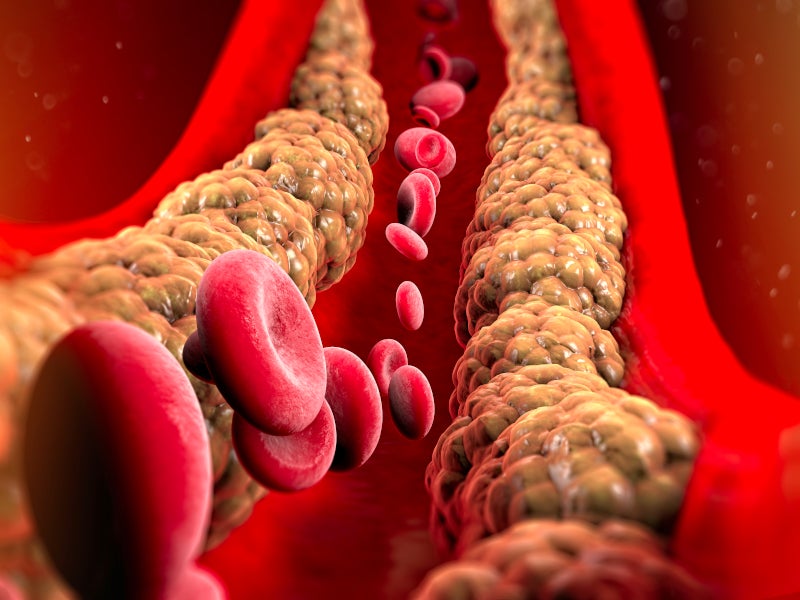
ASMD causes lipids to accumulate in body tissue, which damages the cell and causes cell death, impairing organ functions and damaging organs such as the lungs, spleen and liver.
ASMD is a potentially life-threatening spectrum of disease, with types A, B, and A/B being an intermediate form with varying degrees of CNS involvement.
Signs and symptoms of ASMD can include an enlarged spleen or liver, difficulty in breathing, lung infections, and unusual bruising or bleeding. Palliative and supportive care are currently used to manage the disease’s symptoms.
Xenpozyme’s mechanism of action
Xenpozyme is a recombinant human ASM that replaces the patients’ faulty enzyme and reduces sphingomyelin (SM) accumulation in the patient’s organs. This reduces the accumulation of fat within the cell, as well as some symptoms of ASMD.
Clinical trials on Xenpozyme
The approvals of Xenpozyme were based on positive results from the ASCEND and ASCEND-Peds clinical trials, which enrolled both children and adults.
The ASCEND clinical trial was conducted to evaluate the drug’s efficacy and safety in patients with ASMD type A/B or type B. A total of 36 patients were randomised to receive either Xenpozyme or placebo for 52 weeks.
The study’s primary endpoint was the improvement in the lung’s diffusing capacity for carbon monoxide (DLco) and spleen size reduction. Patients treated with Xenpozyme achieved a 22% improvement in DLco, compared with 3% for patients in the placebo group at week 52.
At week 52, patients treated with Xenpozyme had had a reduction in spleen size by 39.5%, compared with a 0.5% increase for the patients in the placebo group. All ASCEND patients treated with Xenpozyme showed improvement in one or both primary endpoints.
The single-arm ASCEND-Peds clinical trial evaluated 20 paediatric patients with ASMD type A/B or type B. Patients received Xenpozyme with a primary objective to evaluate the drug’s safety and tolerability for 64 weeks. All patients completed the study and continued in an extension trial.
At 52 weeks, a 33% mean increase in DLco was reported in nine patients from the baseline, while the spleen volume mean decrease was 49% from the baseline.
Common adverse reactions reported in both clinical trials were headaches, nasopharyngitis, upper respiratory tract infections, and coughs.