Ovarian cancer has long posed a significant public health challenge given the limited opportunities for early detection. However, treatment has vastly improved in the past decades, reducing mortality and improving patient quality of life. In a recent publication in the Journal of the American Medical Association (JAMA), Gupta and colleagues consider access to ovarian cancer treatment in the US, with a focus on racial and ethnic disparities underlying its treatment, using metrics for healthcare access in conjunction with epidemiological data. Their results assert that race plays a critical role in the patient experience through lower rates of clinical care and more frequent Stage IV diagnoses among racial minorities.
In the US, GlobalData epidemiologists forecast a decline in the diagnosed incidence (cases in every 100,000 of the population) and a stable five-year diagnosed prevalence of ovarian cancer in the coming years. Although these figures show encouraging signs for the management of ovarian cancer, Gupta and colleagues emphasise that clinical outcomes face an equity gap.
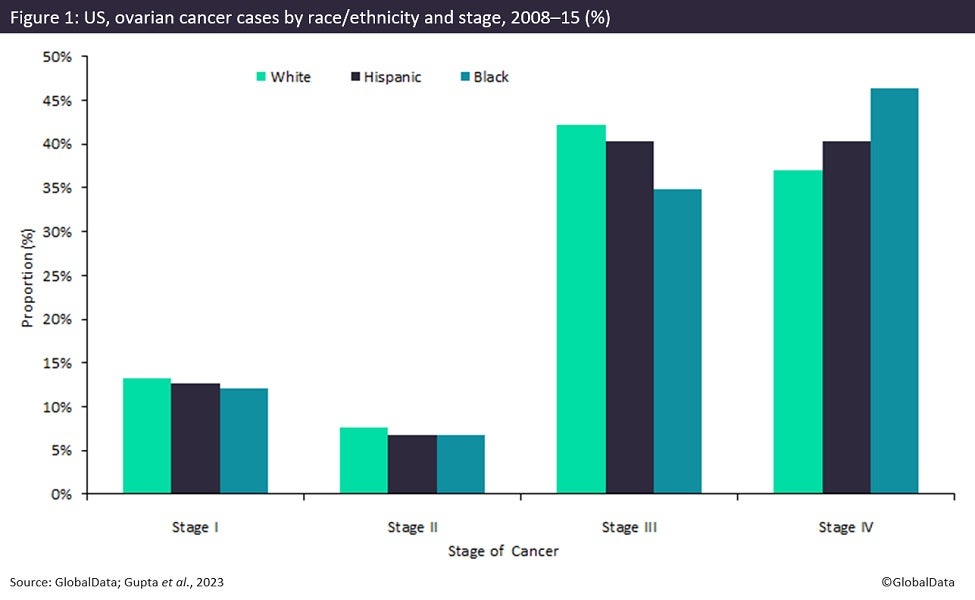
Using patient data from the Surveillance, Epidemiology and End Results (SEER) database, Gupta and colleagues observed Medicare claims among 8,987 women older than 65 years between 2008–15 from 12 US states. This data was segmented by race, location, and stage at diagnosis. Patient outcomes and epidemiology were evaluated against indicators of healthcare access using 35 metrics of affordability, accessibility, or availability of care. Analysis revealed significant racial disparities within several clinical indicators. As seen in Figure 1, 46.4% of Black patients were diagnosed with Stage IV ovarian cancer, compared to 40.3% of Hispanic and 37.1% of white women. The authors found similar gaps in the care that patients received. While 54.8% of white patients reported a consultation with a gynaecological oncologist, only 45.1% of Black patients and 46.8% of Hispanic patients did the same. Likewise, 50.3% of Black women received oncological surgery compared to 59.5% of Hispanic women and 61.7% of white women.
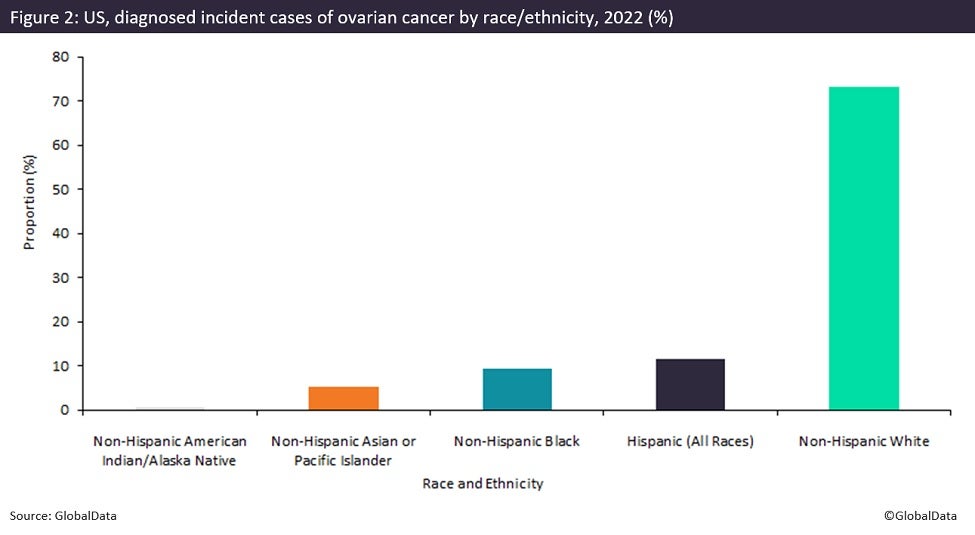
The data highlighted by the authors show a stark racial disparity in care and detection, especially when considered against the racial distribution of diagnosed incident cases of ovarian cancer. As displayed in Figure 2, the majority of cases in 2022 occurred among non-Hispanic white women (73.16%), followed by Hispanic (11.63%) and Black patients (9.30%). Although Black and Hispanic patients compose a lower proportion of cases relative to non-Hispanic white patients, the higher rate of late-stage diagnoses in these groups has significant implications for survival and quality of life. Gupta and colleagues attribute the majority of these inequities to economic inequality but propose that structural racism and implicit biases among healthcare providers may play exacerbating roles.
Against the backdrop of encouraging strides in ovarian cancer care, Gupta and colleagues highlight a more complex picture of the social dynamics underlying the epidemiological trends. GlobalData epidemiologists estimate that diagnosed incident cases of ovarian cancer in the US will decline from almost 22,800 cases to nearly 22,300 cases between 2022 and 2028. Meanwhile, five-year diagnosed prevalent cases show a modest decrease from more than 70,800 to approximately 69,900 cases during the same period. On the one hand, ovarian cancer’s declining incidence rate suggests advances in diagnosis, prevention, and treatment. However, these accomplishments are not distributed equally, and may split along racial and socioeconomic lines.
The remedy to persisting racial disparities in healthcare is both multivariate and structural in scale. The most direct impact could be enacted by improving access to ovarian cancer-related prevention and care among marginalised communities via expanded coverage or discounted care. Furthermore, improving cultural competency among healthcare providers through a more diverse workforce and education can reduce biases in clinical settings. If implemented, these and other changes can expand and bolster the improving landscape of ovarian cancer in the US.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData