Cardiovascular disease (CVD) is a medical term encompassing conditions affecting the heart and circulation. There is a long-established link between people with diabetes and an increased risk of developing CVD. However, it was not until recently that the sex-specific differences in risk across the full glycemic spectrum were quantified in a UK-based research study by Christopher T Rentsch and colleagues.
This large-scale observational cohort study using data from UK Biobank was undertaken with the aim of examining the differences in incident adverse CVD outcomes in men and women in relation to baseline glycated haemoglobin levels. The study, published in The Lancet in 2023, recruited 195,752 men and 231,682 women ages 40–69 years between 2006 and 2010 across England, Scotland, and Wales.
Participants had their baseline glycated haemoglobin (HbA1c) levels measured and then categorised using standard clinical cut-off points into five groups: low-normal, normal, pre-diabetes, undiagnosed diabetes, and diagnosed diabetes. Six CVD outcomes were measured: coronary artery disease (CAD), atrial fibrillation, deep vein thrombosis (DVT), pulmonary embolism (PE), stroke, and heart failure. The study found that both men and women in higher HbA1c groups had more negative health associations, such as higher body mass index, poorer renal function, and greater prevalence of hypertension compared to their counterparts with low-normal or normal HbA1c levels. Compared to their normal HbA1c counterparts, women with pre-diabetes were 1.47 times more likely to be at risk of CVD and women with undiagnosed diabetes were 1.33 times more likely to be at risk. In men, the pre-diabetes group was 1.30 more likely to be at risk of CVD compared to the normal HbA1c group, and the undiagnosed diabetes group was 1.31 more likely to be at risk. Both men and women with low-normal HbA1c were at similar decreased risk of CVD.
Men and women with diagnosed diabetes were more at risk of developing CAD, stroke, and heart failure compared to their counterparts with normal HbA1c. In the mentioned CVD outcomes, women were at higher risk of developing CAD and heart failure, and the risk of developing stroke was the same in men as in women. Having low-normal HbA1c was slightly more protective against the risk of CAD for women than men, although the difference is minimal. Notably, women with diagnoses of diabetes had more of an excess of adverse risk factors compared to men, particularly for adverse waist-to-hip ratio and obesity.
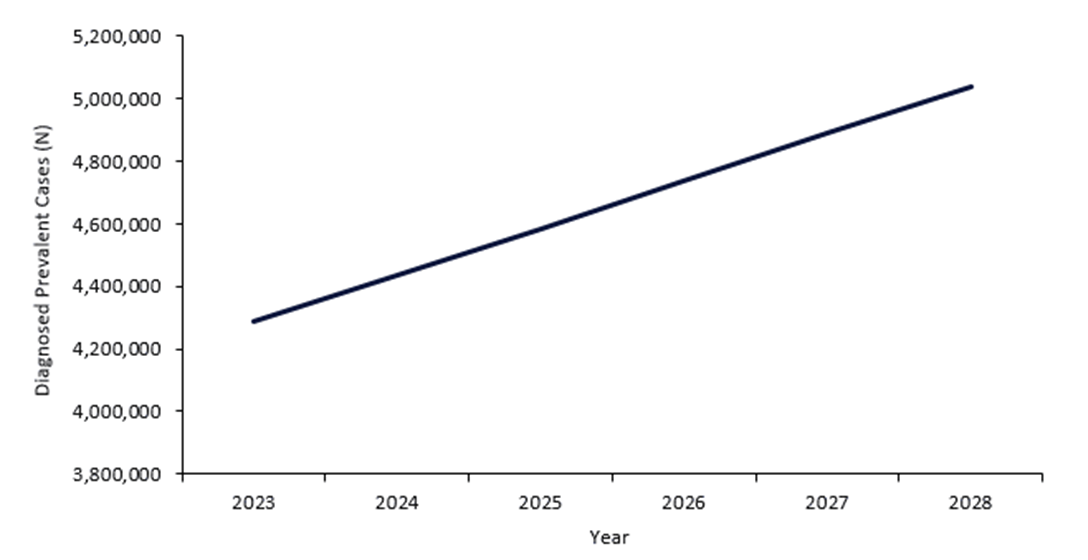
Addressing the issue of an already large population of diabetic men and women, which has been steadily growing since the 1980s, is important for preventing continued health burdens associated with CVD and diabetes. GlobalData epidemiologists predict that in the UK alone, there will be 4.2 million cases of diagnosed prevalent cases of type 2 diabetes in men and women by the end of 2023. That number is forecasted to rise to five million by the end of 2028 (Figure 1, above). This study shows that having abnormally high levels of HbA1c most notably increases the risk of CAD, stroke, and heart failure. However, despite being of the same HbA1c categories, men and women experience the risk of CVD differently, which could be taken into consideration by public health policymakers when they decide to implement prevention strategies to reduce CVD incidence by decreasing the incident cases of pre-diabetic or undiagnosed diabetic individuals.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData