An expanding body of research has shed light on racial disparities in the health outcomes of patients with neurodegenerative diseases.
In a notable addition to this work published in JAMA Open Network, Estrada and colleagues examined the incidence of potentially avoidable hospitalisations (PAHs), which may occur due to inadequate, delayed, or neglectful treatment, in a nationally representative cohort of nursing home residents.
Their analysis indicates that the likelihood of incident PAHs was higher among residents belonging to historically disadvantaged racial and ethnic groups, especially among those living with impaired cognitive function.
Leading data and analytics company GlobalData‘s epidemiologists project an increase in the diagnosed prevalent cases of Alzheimer’s disease (AD) from more than 2,440,000 in 2024 to nearly 2,700,000 in 2028.
The growing prevalence of AD and other age-related neurodegenerative diseases highlights the need for health equity among Americans living in nursing homes and long-term care facilities.
Estrada and colleagues’ analysis utilised four national datasets covering Medicare beneficiaries and long-term care facility records collected in 2018.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataDatasets yielded results for 2,098,285 nursing home residents over 65 years old, 53.6% of whom experienced mild to severe cognitive impairment as measured by the cognitive function scale.
Residents’ medical records were flagged for episodes of hospitalisation that occurred without prior hospitalisations due to the same cause.
Hospital admissions for a wide variety of causes, ranging from congestive heart failure and hypertension to altered mental status, were classified as potentially avoidable.
When adjusted for other demographic attributes, PAHs had a higher probability of occurrence among nursing home residents identified as historically marginalised races and ethnicities compared to White peers.
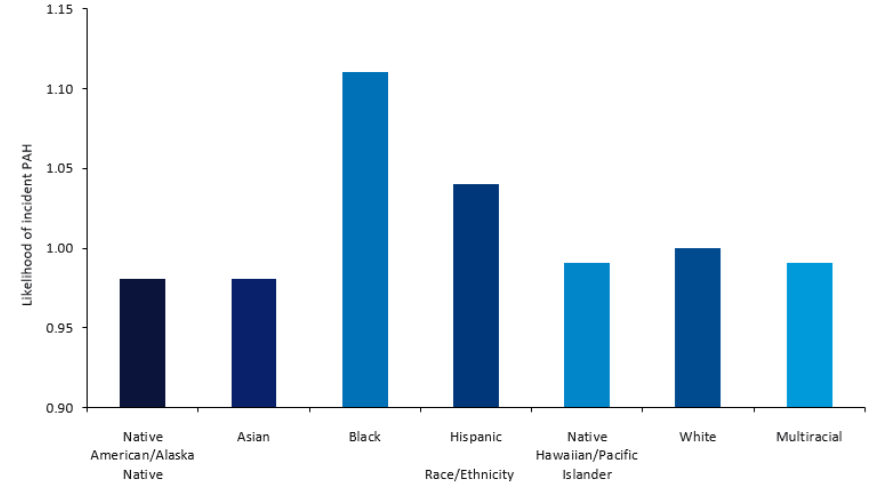
As displayed in Figure 1, Black residents with cognitive impairment were 1.48 times more likely to experience PAHs than their White counterparts, followed by Native Americans and Alaska Natives at 1.43.
Native Hawaiians, Pacific Islanders, and White participants, by contrast, showed the lowest rate of PAHs.
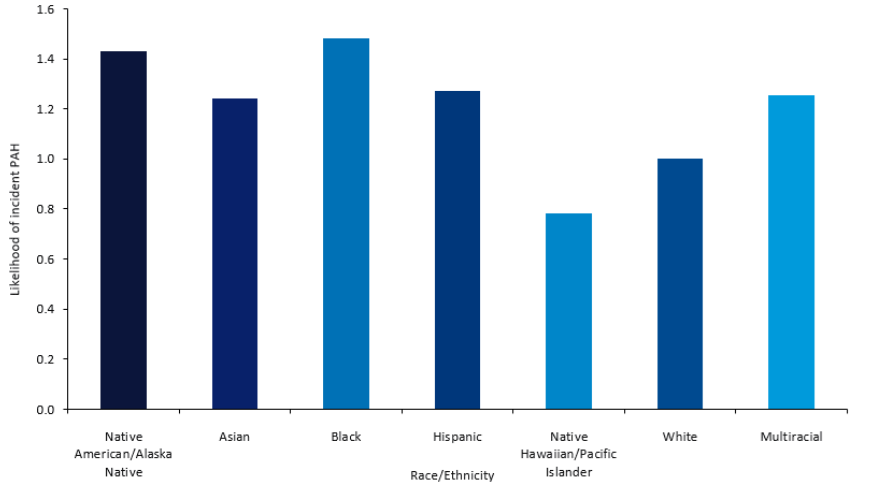
Among residents without cognitive impairment, Black residents also displayed the highest probability of incident PAH at 1.11, with Hispanic residents showing the second highest rate at 1.04 (Figure 2).
The authors propose that differential care practices in facilities, residents’ difficulty communicating pain or distress, and the burden of preexisting illness that may also correlate with race, could have contributed to these results.
In order to address the disparities observed in the study, Estrada and colleagues urge further investigation of PAHs among racial and ethnic minorities, as well as a greater emphasis on equity in nursing home operation policies dictated by US national and state bodies, namely the Centers for Medicare & Medicaid Services.
Such proposals are part of a demand for emphasis on the historical and sociocultural forces that shape health outcomes for marginalised populations.
Within the context of nursing homes, this could take the form of culturally sensitive and specialised care plans, further training of staff members, and more intensive screening for PAHs among minorities with a higher propensity for certain PAHs in older adulthood.
As the American population structure becomes both more diverse and older, these considerations may occupy an increasingly important role in the future of care for the older generation.