Columvi (glofitamab-gxbm) is a bispecific antibody indicated for the treatment of adults with relapsed or refractory (r/r) diffuse large B-cell lymphoma (DLBCL), not otherwise specified (NOS) or large B-cell lymphoma (LBCL) originating from follicular lymphoma, following two or more lines of systemic therapy.
Genentech, a subsidiary of the Swiss pharmaceutical company Roche, developed the drug, which is the first and only fixed-duration bispecific antibody treatment for the condition.
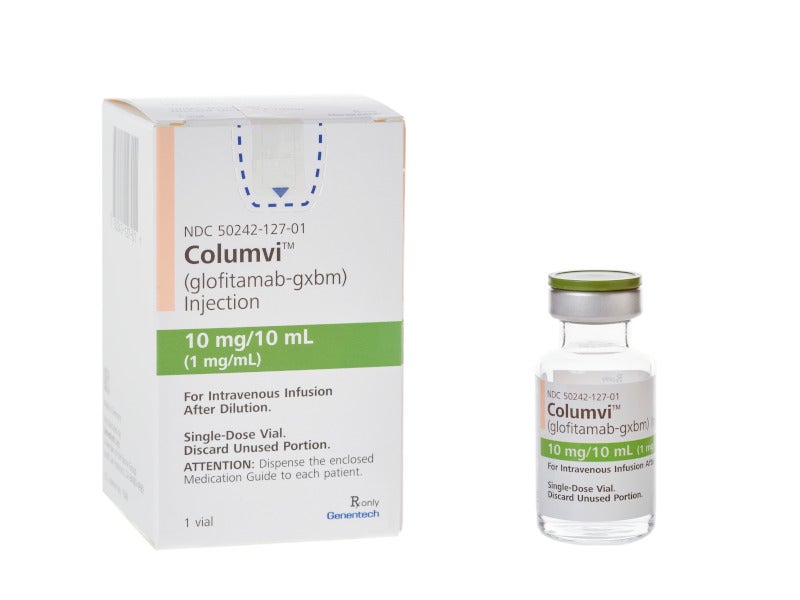
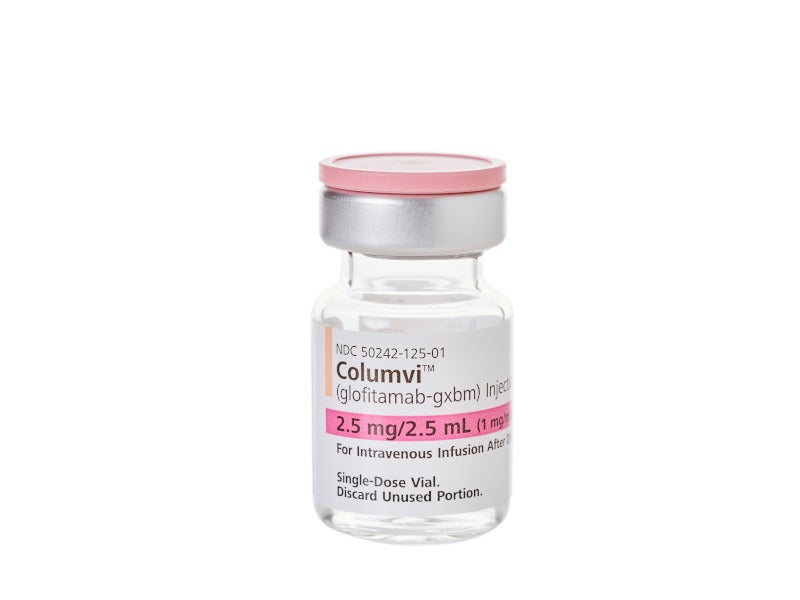
Columvi is available as a colourless and clear solution of 2.5mg/2.5mL and 10mg/10mL strengths in a single-dose vial for intravenous administration.
Regulatory approvals for Columvi
Columvi was granted orphan medicine designation by the European Medicines Agency for the treatment of DLBCL in October 2021.
The drug received its first worldwide approval with conditions in Canada in March 2023.
The US Food and Drug Administration (FDA) approved Columvi under accelerated approval in June 2023, while the European Commission approved the drug in July 2023.
The drug was provisionally approved with obinutuzumab pre-treatment for the treatment of adult patients with r/r DLBCL after two or more lines of systemic therapy in Australia, in August 2023.
DLBCL causes and symptoms
DLBCL is a fast-growing blood cancer and the most prevalent form of non-Hodgkin’s lymphoma (NHL) in the US. It originates in lymphocytes, a type of white blood cells that defend against infections.
DLBCL is a result of B-cell mutations caused by factors such as specific viruses, Epstein-Barr virus, human immunodeficiency virus (HIV), hepatitis B and C virus, post-transplant immunosuppressants, autoimmune conditions, immunodeficiency, high body mass index in youth, agricultural pesticides and ionising radiation.
The symptoms primarily include swollen lymph nodes in the neck, armpit, or groin with fever and sudden weight loss. DLBCL is more prevalent in males compared to females.
Columvi’s mechanism of action
Columvi is a CD20-directed CD3 T-cell engaging bispecific monoclonal antibody, whose two regions bind to CD20 expressed on the surface of B cells which can be healthy or cancerous and one region to CD3 receptor expressed on the surface of T cells.
The dual interaction brings the T-cell close to the B-cell, triggering the release of cancer cell-killing proteins from the T-cell and leading to the death of B cells.
Clinical trials on Columvi
The FDA’s accelerated approval for Columvi was based on positive outcomes from the Phase I/II, multi-cohort, open-label, multi-centre, single-arm clinical trial NP30179 that enrolled 155 patients.
The NP30179 trial was conducted to evaluate the safety, efficacy, tolerability and pharmacokinetics of escalating doses of glofitamab as a monotherapy and in combination with obinutuzumab following a fixed, single-dose pre-treatment of obinutuzumab in patients with r/r B-cell NHL.
The main efficacy outcome measures were objective response rate (ORR) and duration of response (DOR), which were evaluated in 132 patients who received Columvi for a fixed duration of 8.5 months.
The patients achieved durable remission with an ORR of 56%, while 43% achieved a complete response. The median DOR was 1.5 years (18.4 months).
The most common adverse reactions observed in patients during the treatment were cytokine release syndrome (CRS), musculoskeletal pain, rash and fatigue.
The drug’s approval in Europe was based on positive findings from a pivotal cohort in the Phase I/II NP30179 clinical trial. The patients with r/r DLBCL received a fixed course of Columvi treatment in the study, which induced early and long-lasting responses in patients.
In the study, a complete response was achieved in 35.2% of patients, while 50% of patients achieved an overall response. About 74.6% of those who achieved a complete response continued to experience a response at 12 months, although the median duration of a complete response was not reached.