PENBRAYA™, a meningococcal A, B, C, W, and Y vaccine, is indicated for active immunisation to prevent invasive disease caused by Neisseria meningitidis (N. meningitidis) serogroups A, B, C, W, and Y in individuals aged from ten to 25 years.
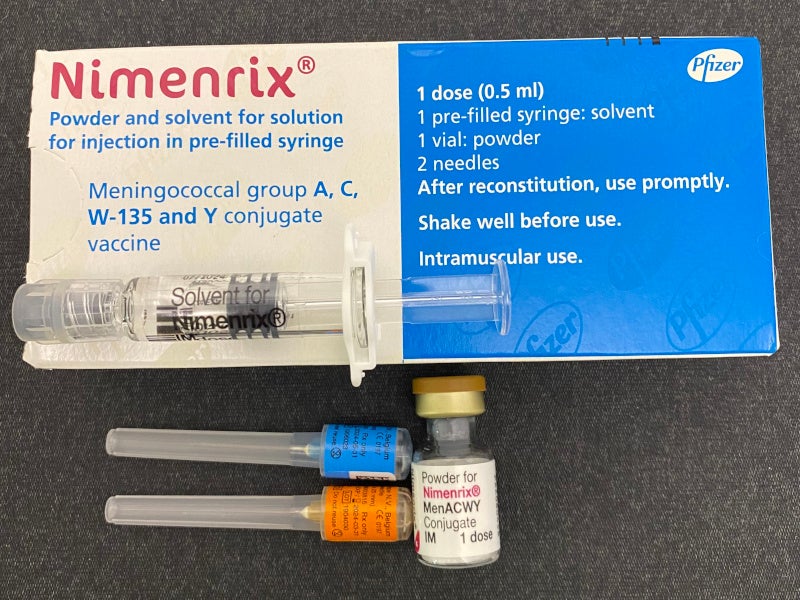
Developed by Pfizer, a biopharmaceutical company based in the US, PENBRAYA is a combination of components from two meningococcal vaccines, Nimenrix® (meningococcal groups A, C, W-135, and Y conjugate vaccine) and Trumenba® (meningococcal group B vaccine), to protect against the majority of invasive meningococcal disease ((IMD) globally.
The US Food and Drug Administration (FDA) approved PENBRAYA in October 2023, following the acceptance of a biologics licence application (BLA) in December 2022.
The Advisory Committee on Immunisation Practices (ACIP) of the US Centres for Disease Control and Prevention (CDC) recommended PENBRAYA for the prevention of the five most common meningococcal serogroups causing most of the IMD in adolescents and young adults of 16 to 23 years of age, in October 2023.
PENBRAYA is a suspension for injection that is supplied as a sterile lyophilised MenACWY component in a vial to be reconstituted with the sterile liquid MenB component in a pre-filled syringe, forming a single vaccine dose of approximately 0.5ml. It is administered as a two-dose series with each dose given six months apart.
Meningococcal disease causes and symptoms
Meningococcal disease is an illness resulting from the N. meningitidis bacteria. While it is uncommon, it can cause severe infections of the brain, spinal cord (meningitis), and bloodstream. Approximately one in ten people carry the bacteria without illness, known as being “a carrier”. The bacteria can, however, invade the body, leading to meningococcal disease. Six serogroups of N. meningitidis, A, B, C, W, X, and Y cause most disease globally. Three of the serogroups, B, C, and Y, cause most of the illnesses seen in the US.
The most common types of symptoms of meningococcal infections include fever, stiff neck, headache, confusion, and increased sensitivity to light. Babies may show symptoms, such as being slow or inactive, irritable, vomiting, feeding poorly, or having a bulging anterior fontanelle.
PENBRAYA’s mechanism of action
PENBRAYA protects against IMD, primarily through complement-mediated antibody-dependent killing of N. meningitidis.
The vaccine is designed to induce the production of bactericidal antibodies that target the capsular polysaccharides of N. meningitidis serogroups A, C, W, and Y, as well as the Factor H-binding protein (fHbp) subfamily A and B variants of N. meningitidis group B.
The effectiveness of PENBRAYA against group B meningococci depends on the antigenic similarity between the vaccine antigen’s fHbp subfamily A or B and the fHbp protein expressed by the bacterial strain, as well as the level of fHbp present on the bacterial surface.
Benefits of PENBRAYA
PENBRAYA has been recognised for reducing the total number of injections required for individuals to achieve full vaccination against meningococcal serogroups A, B, C, W, and Y.
The simplification of the vaccination process aligns with the standard of care and could potentially enhance vaccine uptake. The CDC mentions that combining vaccines into fewer injections may increase the chance of adolescents and young adults receiving their recommended vaccines quickly. Timely vaccination is crucial for minimising delays in acquiring protection against serious diseases.
The broader consequences of routine PENBRAYA usage include a potential reduction in the incidence of IMD, as well as a decrease in the mortality associated with the disease. Furthermore, it could lead to a lower rate of long-term health complications experienced by survivors of the infection.
Clinical trials on PENBRAYA
The FDA’s approval of PENBRAYA was based on data from a Phase II non-controlled and two Phase III active-controlled clinical trials.
The Phase III Study 1 (NCT04440163) and Study 2 (NCT03135834) were both active-controlled, observer-blinded, multi-centre studies conducted in the US and Europe, involving participants aged ten to 25 years who were MenB vaccine-naive.
In Study 1, 1,763 participants received at least one dose of PENBRAYA while 650 received Trumenba, at zero and six months.
In Study 2, 543 participants were administered PENBRAYA and 1,057 received Trumenba following the same schedule.
In both the studies, GSK’s Menveo® (meningococcal groups A, C, Y, and W-135 Oligosaccharide Diphtheria CRM197 Conjugate Vaccine (MenACWY-CRM)) was co-administered with Trumenba at month zero. The studies included both MenACWY conjugate vaccine-naive and MenACWY conjugate vaccine-exposed participants.
The primary objective of the studies was to establish the immunologic non-inferiority of the pentavalent vaccine candidate in comparison to the currently licensed meningococcal vaccines in the US.
The trials demonstrated that PENBRAYA’s immunogenicity was non-inferior to Trumenba + Menveo for all serogroups and had a well-tolerated safety profile.
The Phase II trial constituted a descriptive, non-controlled study wherein participants aged 11 to 14 years in the US were administered PENBRAYA at 12-month intervals. All participants had no prior exposure to any meningococcal vaccine.
The findings from the three trials showed robust immunogenicity of PENBRAYA that is non-inferior to the combination of Trumenba and Menveo for all serogroups under consideration. Furthermore, the vaccine was well-received by the trial participants, displaying a favourable safety profile.
The most common adverse reactions were pain at the injection site, fatigue, headache, redness at the injection site, muscle pain, swelling at the injection site, joint pain, and chills.
Other significant meningococcal conjugate vaccines in the market
Before PENBRAYA, there were no licensed pentavalent meningococcal conjugate vaccines available in the US for active immunisation against IMD caused by N. meningitidis serogroups A, B, C, W, and Y.
Quadrivalent vaccines such as GSK’s Menveo and Sanofi’s Menactra and MenQuadfi are available for different age groups, with specific dosing schedules. Pfizer’s Nimenrix is licensed in Europe for individuals aged six weeks and older.
In the US, serogroup B vaccines, including Pfizer’s Trumenba and GSK’s BEXSERO, are available for individuals aged ten to 25 years, with specific dosing regimens. The FDA approved Trumenba in October 2014.
Trumenba and Nimenrix have been available in the European market since 2017 and 2012, respectively.