The product of a joint development programme between Sanofi-Aventis (formerly Sanofi-Synthelabo) and Organon, Idraparinux is a new addition to the synthetic oligosaccharide family of anticoagulant drugs. It is indicated for the treatment and secondary prevention of venous thromboembolism (VTE), as well as the prevention of thromboembolic events associated with atrial fibrillation.
In early 2004, Sanofi-Aventis assumed full responsibility for the development of idraparinux. This followed a decision to reacquire all rights to the family of synthetic oligosaccharide agents, which include not only idraparinux, but also the already licensed agent, Arixtra.
Subsequently, the company divested its interest in arixtra (fondaparinux sodium) and its LMWH Fraxiparine (nadroparine calcium) to GSK as a condition of the formation of Sanofi-Aventis. In acquiring arixtra, GSK has also assumed responsibility for any ongoing arixtra clinical trials.
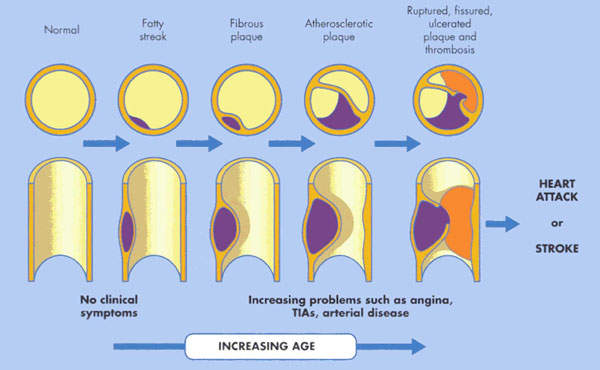
VTE (venous thromboembolism) constitutes a major medical problem
VTE encompasses deep-vein thrombosis (DVT) and pulmonary embolism (PE). It is the third most common cardiovascular disease after heart attack and stroke.
In the US alone, it is estimated that two million people are affected by VTE. Of these, 60,000 die from PE, which occurs when a clot in the deep veins of the leg breaks away and becomes lodged in the pulmonary artery. VTE is often asymptomatic.
Patients undergoing major orthopaedic surgery (hip or knee replacements, hip fracture) are at an especially high risk of developing VTE.
Without anticoagulant therapy, between 40% and 50% of patients undergoing hip replacement surgery suffer VTE. This rises to 70% to 80% in hip fracture surgery.
Antithrombotic agents used to prevent blood clots
Launched in the US and Europe in 2002, arixtra was thes first in a new class of antithrombotic agents: selective inhibitors of coagulation Factor Xa.
Inhibition of Factor Xa interrupts the coagulation cascade at the critical point where the intrinsic and extrinsic pathways meet and so prevents the formation of blood clots. Via selective and potentiated ATIII-mediated inhibition of Factor Xa, arixtra produces rapid and predictable antithrombotic activity at very low doses.
Unlike the low molecular weight heparins with which it competes in the cardiovascular market, arixtra is a totally synthetic product. This ensures purity of product, predictable pharmacokinetics and batch-to-batch consistency.
In common with arixtra, idraparinux also selectively inhibits coagulation Factor Xa. However, its potency and long duration of action enable it to be given as a single weekly injection, a significant therapeutic advance.
There is no evidence that it interacts with foods or drugs, which is a known drawback with oral agents such as warfarin.
Comparison with existing anticoagulant treatments on the market
PERSIST, a Phase II dose-ranging study, was completed in 2002. The trial compared idraparinux with current oral anticoagulant treatments in protection against recurrent VTE. Results showed that, at a dose of 2.5mg, idraparinux was at least as effective as existing treatments in VTE prevention, with potential advantages in both safety and patient convenience.
On the basis of successful dose-ranging Phase II trials, idraparinux progressed to Phase III development, where it was evaluated in more than 10,000 patients.
Phase III trials of idraparinux tested its effectiveness in the treatment of DVT and PE together with efficacy and safety in long-term prevention of stroke in patients suffering from atrial fibrillation.
The Phase III AMADEUS trial was designed to demonstrate that idraparinux is at least as effective as oral dose-adjusted anticoagulant therapy but provides superior safety in the long-term prevention of thromboembolic events associated with atrial fibrillation.
Data released in 2007 showed, however, that while it was as effective as vitamin-K antagonists (warfarin), it caused significantly more bleeding.
In fact, the trial was stopped early after randomisation of 4,576 patients and a mean follow-up of 10.7 months due to excessive clinically relevant bleeding in the idraparinux treatment arm. Excess bleeding, which was most notable in elderly patients and those with renal impairment, involved both intracranial and other haemorrhages.
Phase III trials (Van Gogh PE, Van Gogh DVT and Van Gogh Extension)
Three new comparative Phase III trials were started (Van Gogh PE, Van Gogh DVT and Van Gogh Extension) focusing on the long-term treatment of patients with confirmed DVT or PE.
The studies compared idraparinux with standard oral anticoagulant therapy, with the trials designed to demonstrate that idraparinux is at least as effective as standard agents but superior in safety.
In December 2006, Sanofi announced mixed results from its Van Gogh studies. The original study, which included 2,904 patients, achieved its primary end point. After three months, significantly fewer clinically relevant bleedings were witnessed during the trial.
The Van Gogh PE study, which included 2,215 patients, did not meet the primary end point in the first three months and showed an increase in the mortality rate.
The Van Gogh Extension trial, which included 1,215, patients achieved its primary end point and demonstrated lower rate of major bleedings in the active arm after six months. Sanofi now plans to file for approval for the drug.
Sanofi has developed a modified version of idraparinux, idraparinux biotinylated, which is similar to its predecessor but contains a biotin segment. The clinical development of the drug was designed in such a way as to bridge with the clinical results obtained with idraparinux.
Two bioequipotency studies in patients suffering from deep vein thrombosis and pulmonary embolism, EQUINOX and CASSIOPEA, were started in 2006.
The EQUINOX trial enrolled 757 patients and was completed in January 2008. It evaluated the safety and efficacy of biotinylated idraparinux with that of idraparinux. Results from the study indicated that biotinylated idraparinux had a similar efficacy when compared with idraparinux alone.
The CASSIOPEA study compared biotinylated idraparinux with warfarin. The trial enrolled 3,200 patients and was completed in October 2010.
A Phase III study, BOREALIS-AF, was started in 2007 to compare the safety and efficacy of the drug versus vitamin K antagonists in patients suffering with atrial fibrillation. The study, however, was terminated although the decision was not based on safety concerns.
Marketing commentary for antithrombotic agents / anticoagulant treatments such as arixtra and idraparinux
Standard anticoagulants include oral anticoagulants, such as the vitamin K antagonist warfarin and aspirin, as well as injectable heparins, such as enoxaparin.
Although they have all proved valuable in VTE prophylaxis, there remains a need for new agents, epitomised by idraparinux’s predecessor arixtra. Ideally, new anticoagulants need to be:
– More effective but without increasing the risk of bleeding
– Rapid and predictable in action
– More convenient to administer
– Fixed dose without the need for regular monitoring
– Cost-effective in the prevention of VTE
Idraparinux shares many of the properties of arixtra but has the added advantage of a highly convenient once-a week dosing regimen.
Available anticoagulants have to be taken daily. Idraparinux remains part of the Sanofi-Aventis development pipeline following the divestment of arixtra to GSK.