NGENLA® (somatrogon) is a once-weekly, long-acting therapy created using recombinant technology for paediatric patients aged three years and older, who experience growth failure due to an inadequate secretion of endogenous growth hormone.
Opko Health, a US-based healthcare company, developed the drug as a long-acting human growth hormone (hGH-CTP) for the treatment of paediatric and adult growth hormone deficiency (GHD).
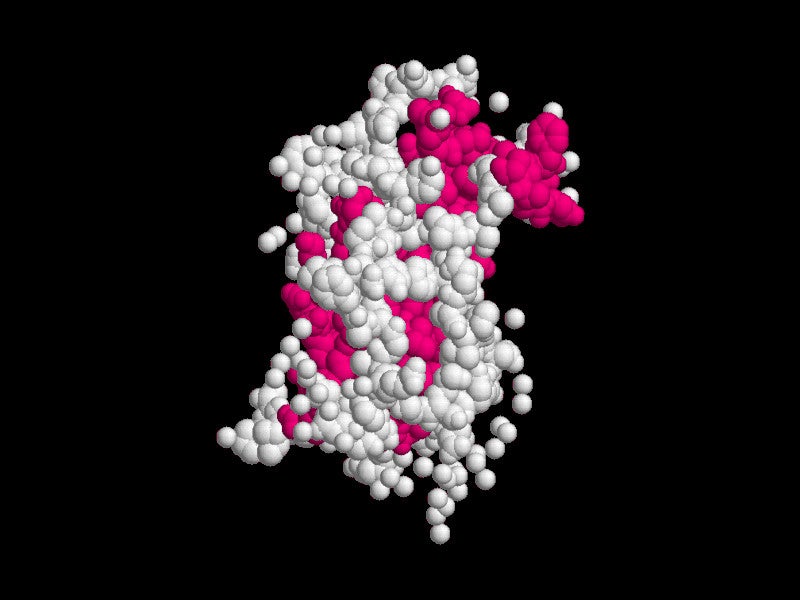
OPKO utilises its exclusive technology to prolong the half-life of hormones without relying on polymers, encapsulation methods, or nanoparticles. The foundation of the technology lies in a natural peptide known as the C-terminal peptide (CTP) derived from the beta chain of human chorionic gonadotropin (hCG).
Opko Health entered a global agreement with US-based biopharmaceutical company Pfizer to further develop and commercialise the drug for the treatment of GHD in both adults and children in December 2014. Additionally, the partnership aims to address growth failure in children born small for gestational age (SGA) who do not exhibit catch-up growth by the age of two years.
The NGENLA is a clear, colourless to slightly light-yellow solution. It is available in single-patient-use, disposable prefilled pen doses of 24mg/1.2ml (20mg/ml) and 60mg/1.2ml (50mg/ml). The pens allow for incremental dosing adjustments of 0.2mg and 0.5mg, respectively, for subcutaneous administration.
Advantages of NGENLA over traditional growth hormone therapies
The molecule combines the natural peptide sequence of native growth hormone with the 28 amino acids of the CTP. It aims to decrease the frequency of injections for growth hormone replacement therapy in children and adolescents with GHD from a daily regimen to once a week, offering a more convenient treatment option.
Its extended action in the body indicates that patients require only weekly injections, a significant improvement over the daily injections required by traditional growth hormone therapies such as GENOTROPIN® (somatropin).
NGENLA is administered subcutaneously through an injection device that allows for precise titration based on patient needs. The drug offers approximately 85% fewer injections, which can be administered any time of the day, not just at night.
Regulatory approvals for NGENLA
The US Food and Drug Administration (FDA) approved NGENLA for the treatment of paediatric GHD in June 2023. The European Commission (EC) had provided marketing authorisation (MA) to the drug in February 2022.
Japan’s Ministry of Health, Labour, and Welfare (MHLW) approved NGENLA in January 2022, offering it in both 24mg and 60mg pen options.
NGENLA is currently approved in more than 40 markets such as the UK, Canada, Australia, South Korea, Taiwan, India, and Brazil for the treatment of paediatric GHD.
Growth hormone deficiency causes and symptoms
GHD is a condition marked by insufficient secretion of growth hormone from the anterior pituitary gland, which is crucial for children’s growth and maintaining a healthy balance of muscle, bone, and fat tissues.
The condition can be congenital due to genetic mutations or brain structural defects, or acquired later in life through trauma, infection, radiation therapy, or tumour growth. Some cases have no identifiable cause and are deemed idiopathic.
Paediatric growth hormone deficiency (pGHD) affects approximately one in 3,500 to 10,000 children, leading to delayed or restricted growth. Adult growth hormone deficiency (AGHD) is estimated to affect approximately 50,000 individuals in the US alone.
Symptoms of GHD can include a younger appearance, abdominal fat, thin hair, slow tooth development, poor nail growth, delayed facial bone development, teeth eruption, truncal obesity, and delayed skull closure. In children, pGHD can result in significantly shorter stature compared to peers and is associated with delayed physical development.
NGENLA’s mechanism of action
NGENLA is a novel long-acting human growth hormone receptor (GHR) agonist. It binds to and activates the GHR, which subsequently initiates a series of signal transduction events, triggering changes in growth and metabolism.
The binding causes activation of the STAT5b signalling pathway and the subsequent increase in serum concentration of insulin-like growth factor (IGF-1). GH and IGF-1 are essential for stimulating growth and metabolic functions within the body.
By mimicking the effects of endogenous growth hormone, NGENLA not only promotes linear growth but also enhances protein synthesis and affects the metabolism of carbohydrates, lipids, and minerals.
Clinical trials on NGENLA
The FDA’s approval of NGENLA was based on a multi-centre, randomised, open-label, active-controlled Phase Ⅲ clinical study. The trial’s design aimed to compare the once-weekly administration of NGENLA with the once-daily administration of GENOTROPIN® (somatropin).
A total of 224 treatment-naive, paediatric patients with GDH were randomised in a 1:1 ratio to receive either NGENLA once-weekly at a dose of 0.66mg/kg/day or somatropin once-daily at a dose of 0.034mg/kg/day.
The primary efficacy endpoint of the study was annualised height velocity at week 52.
After 52 weeks of treatment, the group treated with NGENLA exhibited an annualised height velocity of 10.1cm/year. In comparison, the patients who received daily somatropin demonstrated an annualised height velocity of 9.8cm/year at the end of the same treatment period.
The study successfully demonstrated the non-inferiority of NGENLA compared to somatropin. NGENLA was generally well-tolerated by the participants in the study, showcasing a safety profile that was comparable to that of somatropin.
The most common adverse reactions were injection site reactions, nasopharyngitis, headache, pyrexia, anaemia, cough, vomiting, hypothyroidism, abdominal pain, rash, and oropharyngeal pain.